Long-term rate of transvenous lead complications ‘disappointing,’ researchers say
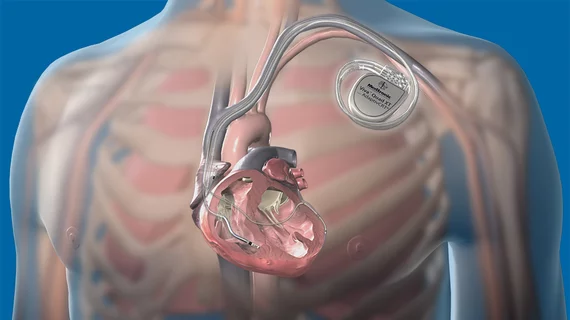
One-fourth of transvenous implantable cardioverter defibrillator (ICD) leads has a mechanical complication within 10 years, according to an insurance database analysis published May 10 in the Journal of the American Heart Association.
A team of researchers from Boston Scientific, which funded the study, and Virginia Commonwealth University studied 40,837 patients who had ICDs or cardiac resynchronization therapy defibrillators (CRT-Ds) implanted from January 2003 through June 2015. Over an average follow-up of 2.3 years, 5.3 percent of the patients who had the devices implanted experienced a mechanical complication and 1.9 percent experienced an infection.
When extended out to five years, the rates of mechanical complications increased to 8.0 percent for ICDs and 10.7 percent for CRT-Ds.
“Lead‐related complications remain a significant cause of morbidity and mortality associated with the transvenous ICD system, in addition to incurring an unacceptably high financial burden for patients, caregivers, and the healthcare system,” wrote lead author Jayanthi N. Koneru, MD, with VCU School of Medicine, and colleagues. “Reliability of ICD leads at five and 10 years continues to be disappointing. Careful consideration should be given to the choice of leads or nontransvenous ICD systems, particularly for patients at a higher risk for mechanical complications or infection.”
Boston Scientific’s involvement in this study is notable because the company is currently marketing its subcutaneous implantable cardioverter defibrillators (S-ICDs), which were developed to reduce complications related to transvenous leads. At the Heart Rhythm Society’s recent scientific sessions, investigators shared results from a study showing an oversensing filter added to the S-ICD cut the risk of inappropriate shocks by more than 50 percent.
In the JAHA analysis, Koneru and coauthors found that subsequent procedures to treat infection and mechanical failure cost $68,000 and $36,000, respectively. In addition, the average cost of care for patients with infectious complications was higher in the years surrounding the follow-up intervention.
“This is in consonance with other studies that suggest that the healthcare expenditure associated with infections and reinterventions could be astronomical,” the researchers noted.
The average age of the study population was 61.7 and 73 percent of the patients were men. Koneru et al. noted men and individuals with diabetes, atrial fibrillation and chronic kidney diseases were more likely to have device-related infections, as well as those with multiple ICD procedures. On the other hand, women and younger patients with fewer comorbidities were more likely to have long-term mechanical lead problems, primarily because they live a longer time with the device implanted.
Mortality information couldn’t be gleaned from the database, which included administrative claims from privately insured and Medicare Advantage enrollees. In addition, device manufacturer and model types were not available, so the researchers were unable to identify patients with devices that were later recalled.