Paroxysmal AFib burden linked to higher stroke risk
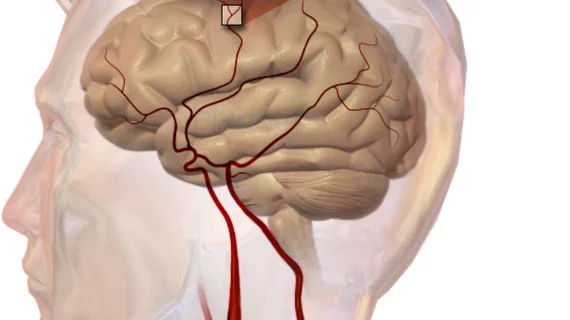
Even for patients with intermittent atrial fibrillation (AFib), the amount of time spent in an arrhythmic state is strongly associated with an increased risk of stroke, researchers reported in JAMA Cardiology.
AFib is a recognized risk factor for stroke, but previous reports have failed to establish whether the burden of paroxysmal AFib is independently linked to thromboembolism.
Lead author Alan S. Go, MD, and colleagues studied nearly 2,000 adults who were found to have at least one episode of AFib during a two-week period of continuous electrocardiographic monitoring. The median amount of time spent in AFib was 4.4 percent, while patients in the top one-third of AFib burden were in arrhythmia at least 11.4 percent of the time they were monitored.
After adjusting for the ATRIA stroke risk score, people in that top tertile demonstrated a 3.13-fold risk of stroke while not taking anticoagulants compared to the rest of the cohort. Each additional hour spent in AFib was associated with a 3 percent increased risk of stroke.
"This study has the potential to have a major impact on heart care," senior author Matthew D. Solomon, MD, PhD, a cardiologist at Kaiser Permanente in Oakland, California, said in a press release. "Using new continuous heart-monitoring technology, physicians can identify patients with intermittently recurring atrial fibrillation at greater risk and engage in better-informed shared decision-making around stroke prevention strategies."
The researchers noted their results were consistent when analyzed across different clinical and demographic subgroups. The average age of the study population was 69 and 55 percent were men. Thromboembolism occurred at an unadjusted rate of 1.51 per 100 person-years.
“Given the number of events, we had limited power to determine thromboembolic risk at more granular cutoffs of atrial fibrillation burden, but our data suggested a threshold of approximately 11 percent as meaningful in the overall cohort and across age, sex and subgroups without diabetes, chronic kidney disease, and hypertension,” Go and colleagues noted.
Considering most patients in the study were at low to medium stroke risk based on validated prediction models, the authors of an accompanying editorial said measuring AFib burden could help to upgrade some of these patients to a higher risk classification.
“In these low-risk patients, increased AFib burden may identify those with additional and actionable stroke risk in whom the net clinical benefit of OAC (oral anticoagulation) is favorable,” wrote Benjamin A. Steinberg, MD, MHS, and Jonathan P. Piccini, MD, MHS. “Given the pervasive and growing use of continuous electrocardiographic monitoring, it is high time for a randomized clinical trial of AFib burden–guided OAC among patients with low CHA2DS2-VASc scores (0-1).”