Real-world Watchman results hold up at 2 years
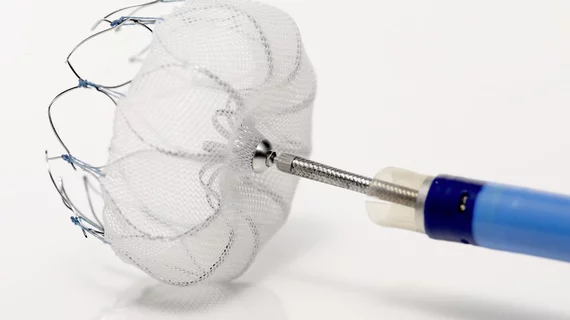
Left atrial appendage (LAA) closure with the Watchman device was associated with low rates of stroke and bleeding events in high-risk atrial fibrillation patients over a two-year follow-up period, according to a real-world analysis published April 3 in Circulation: Electrophysiology and Arrhythmia.
A meta-analysis of two randomized controlled trials found that LAA closure with the Watchman was noninferior to warfarin for preventing stroke and was also associated with lower rates of nonprocedural bleeding and mortality, wrote lead author Lucas V. Boersma, MD, PhD, with St. Antonius Hospital in the Netherlands, and colleagues.
To see whether those outcomes translated to routine clinical practice, the researchers initiated an international registry, called EWOLUTION, of 1,020 patients implanted with the Watchman from 47 different centers. They were 73.4 years old on average and 49% of them had a CHA2DS2-VASc score of 5 or higher—indicating a high risk of stroke.
But after a median follow-up of two years, Boersma et al. observed the following outcomes:
- 22 strokes, or 1.3 per every 100 patient-years, which correlates to an 83% reduction in strokes compared to historic data of the population’s risk profile.
- 47 nonprocedural bleeding events, translating to 2.7 per 100 patient-years—a 46% reduction versus historic data.
- Stroke and bleeding rates were 76% and 41% percent lower, respectively, than historic data would indicate among the 311 study participants with prior ischemic stroke. For the 153 with prior hemorrhagic stroke, stroke and bleeding rates were 81% and 67% lower, respectively.
- Device thrombus occurred in 34 patients (4.1%).
The authors noted these outcomes were achieved despite 72% of patients having a contraindication to oral anticoagulation (OAC).
“During the complete 2-year follow-up … patients with a WATCHMAN left atrial appendage occlusion device had consistently low rates of stroke and nonprocedural bleeding, although most were contraindicated to oral anticoagulation and used only single antiplatelet therapy or nothing,” Boersma et al. wrote.
The nonrandomized nature of this analysis and the lack of a control group were significant limitations, the authors acknowledged. Nevertheless, the real-world results are largely in line with those observed in the device’s randomized controlled trials (RCTs).
“This study represents an EWOLUTION in patient care by extending the positive findings of the Watchman RCTs to a higher risk population (mean CHA2DS2-VAsc score 4.5±1.6) and supports the use of single or dual antiplatelet therapy alone (without OAC) after device implantation,” Srinivas R. Dukkipati, MD, and co-authors wrote in a related editorial. “In the absence of randomized controlled data of OAC contraindicated patients and comparative studies of post-implantation antithrombotic regimens (which we have yet to see), the real-world findings of EWOLUTION may be as good as it gets.”
Boersma and colleagues’ study was funded by Boston Scientific, the manufacturer of the Watchman device.