Smartphone app accurately detects AFib—but 28% of recordings don't suit algorithm
A handheld cardiac rhythm recorder that links to a smartphone application detected atrial fibrillation (AFib) with 96.6 percent sensitivity and 94.1 percent specificity compared to physician-interpreted electrocardiograms (ECGs), according to a single-center study published in HeartRhythm.
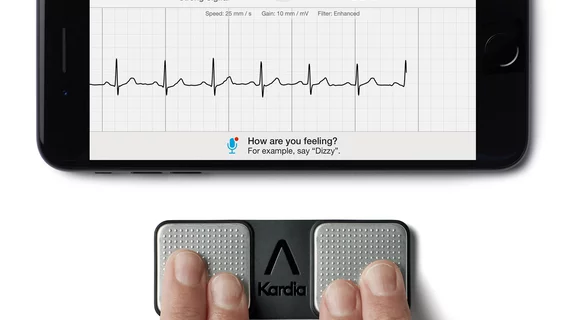
The study included 225 instances in which a 12-lead ECG was recorded almost simultaneously with a 30-second Kardia Mobile Cardiac Monitor (KMCM) rhythm strip.
Similar to recent findings of the Kardia Band smartwatch application, the false negative detection rate shrunk when physicians reviewed the results. Physician-interpreted KMCM recordings demonstrated a 100 percent sensitivity and 89.2 percent specificity for identifying AFib when compared to physician-interpreted ECGs.
"This study is the first independent validation of this smartphone monitor system in the clinical setting using near simultaneous 12-lead ECGs," lead researcher Khaldoun G. Tarakji, MD, MPH, an electrophysiologist with the Cleveland Clinic, said in a press release. “In addition to providing an instantaneous rhythm interpretation, this smartphone monitor system is able to transmit a recording to a secure server where the recordings can be directly reviewed.”
A notable limitation of the technology was the relatively high proportion of unclassified recordings. About 28 percent weren’t able to be categorized as “normal” or “possible AFib” because the readings weren’t suitable for the algorithm. The researchers said most of the unclassified rhythm strips were due to the recordings being less than 30 seconds, the heart rate being too slow (below 50 beats per minute) or too fast (above 100 bpm) or there being too much noise during rhythm capture.
Based on these results, Tarakji said the smartphone algorithm shouldn’t be considered as a substitute for physician analysis. Electrophysiologists reviewed the “unclassified” recordings and detected AFib with 100 percent sensitivity and 79.5 percent specificity against the ECG readings.
“Given its highly accurate performance when able to provide an interpretation, (the algorithm) holds potential as an adjunct to clinical decision making,” he said. “Patients can use an automated AFib detection as a basis for pursuing additional medical follow-up, and clinicians may use it to develop treatment plans supported by more objective data rather than relying only on symptoms.”