Surgery, interventional therapies still the best choice for many HCM patients
Until recently, the rare disease hypertrophic cardiomyopathy (HCM) could only be treated using surgical myectomy or interventional alcohol septal ablation. But that changed in 2022 when the first drug to treat HCM, mavacamten, entered the market. This first noninvasive treatment has created an explosion of interest in HCM and has revised how patients are managed, but alcohol ablation and myectomy still play a key role.
Srihari “Hari” Naidu, MD, director of the cardiac catheterization laboratory and Hypertrophic Cardiomyopathy Center of Excellence at Westchester Medical Center, spoke with Cardiovascular Business about the invasive treatments for HCM. Naidu was among the experts who attended an HCM forum hosted by the American Society of Echocardiography (ASE) in June to hash out what is needed to advance and standardize HCM care.
"There has been a movement toward more invasive therapies over the past 10-15 years. That is because, after surgical myectomy or alcohol septal ablation, we have very good outcomes that show remodeling of the heart, improvement in diastolic function and some observational data that the mortality curves may be improving," Naidu said.
There is also now a belief that earlier interventions may improve HCM patient prognosis over the long term. Experts believe this is better that waiting for patients to be become very sick and begin to go into heart failure before intervening. For this reason, he said many of the top HCM Centers of Excellence have lowered the threshold for when they will use invasive therapies to expand the number of patients eligible.
"You have to look at each patient and understand their goals, what are their motivations, do they want to be own medications or are they having side effects from the medications, and are they adequately controlled. You often have to take that jump and see if you can make them better with the treatments," Naidu explained.
But, he added, invasive therapies all have their own set of risks or issues. Mortality from myectomy is less than 1% and the need for a pacemaker post-procedure is about 5% at experienced HCM centers. Also, anytime you open the body a patient may face complications, or a a period of recovery and rehab he said. Patients in the middle of their career or if they have small children do not want to deal with the possible issues and recovery.
Alcohol septal ablation is less invasive, but also has a mortality rate of less than 1% and a higher pacemaker rate of between 10-20%.
Mavacamten has changed the equation, where patients on the drug may have their hypertrophy controlled and may not need surgery or ablation. Naidu said this appears to be the case for the majority of patients based on recent studies. So the easy answer is that all HCM patients should go on the drug therapy, but he added that things in medicine are rarely that easy.
"There are logistical challenges to the medication, some financial challenges to the medication, and there are reproductive issues with the medication in young people," Naidu explained.
Logistical challenges include how close a patient is to a clinic or hospital so they can receive regular serial echocardiography exams. This is an FDA requirement to prescribe mavacamten to monitor the impact of the drug and to titrate the dose. If patients cannot make regular echo appointments, they cannot receive the medication.
While some patients may not respond to mavacamten, others may be disqualified if their ejection fraction drops too low or they develop heart failure.
Naidu also noted that older patients also might be better off just having the problem of obstruction fixed, rather than going on the drug and having to meet its related echo requirements. An invasive procedure can help the patient avoid the need to take an additional drug and it can eliminate one problem is they have a list of other commodities.
"On the flip side, a young women of prime reproductive age may want a surgical fix and avoid medical therapies where they do not know if there is any fetal toxicity or lactation issues are," Naidu said.
How does myectomy or alcohol septal ablation help HCM patients?
HCM is an inherited disease that causes hypertrophy, which is an increase and growth of heart muscle cells. This increases the size of the myocardium, which can begin to obstruct the left ventricular outflow tract (LVOT) which can lead to heart failure.
Surgical myectomy is an open heart procedure where extra heart tissue is cut off and removed to clear the obstruction.
Catheter-based alcohol septal ablation is less invasive. An interventional cardiologist navigates a catheter to targeted vessels, supplying blood to the septum and injecting alcohol to kill the portion of the myocardium that is causing the obstruction.
New invasive procedures to treat HCM
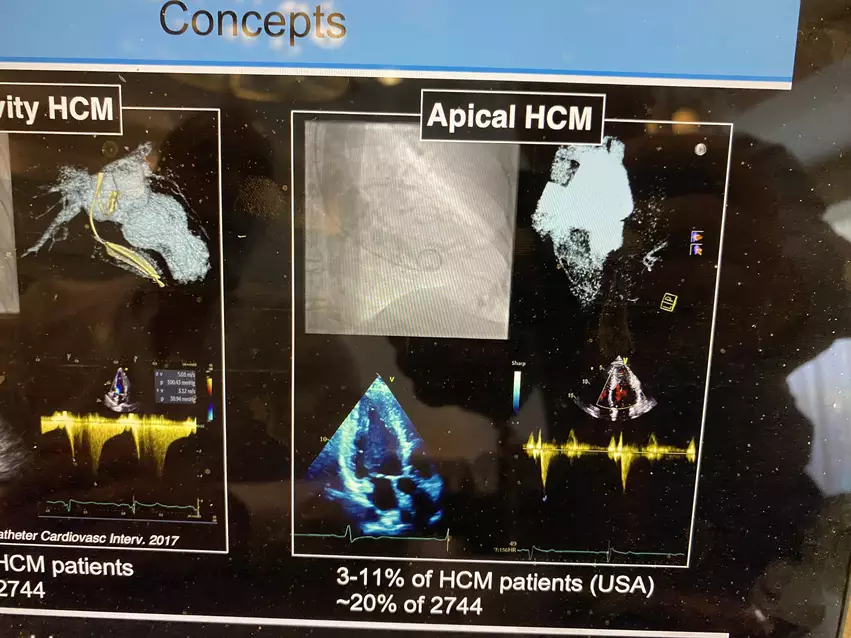
In the surgical realm, research is being done to perform apical myectomies in patients with apical HCM. Another novel technique is beating-heart myectomy, where a biopsy are removed to avoid the need for open heart surgery. Naidu said there are also new procedures to modify the papillary muscle and the mitral valve.
"For interventional techniques, I think the field has moved rapidly because of the advent of structural heart disease interventions. Now that we are looking more at the mitral valve space, we know the transcatheter replacement of that valve often has LVOT obstruction. So there has been a blossoming of technologies to avoid LVOT obstruction and those technologies might be moving into the HCM space," Naidu said.
One technique introduced last year is septal scoring along midline endocardium (SESAME). The transcatheter procedure mimics surgical myectomy by using an electrosurgery wire to cut into the enlarged septum to make more room in the LVOT.
Research is also ongoing to use electrophysiology (EP) ablation catheters to treat the hypertrophic tissue. Another possibility is using an interventional radiology radio-frequency (RF) ablation catheter used to treat liver cancer to ablate the tissue.