Experts hope improved PAD awareness can lead to fewer leg amputations
According to a new national survey released by the PAD Pulse Alliance, 70% of Americans are unaware of peripheral artery disease (PAD), which is the most common vascular disease in the legs and results in the amputation of 400 legs or feet per day in the United States.
Additionally, risk factors for PAD disproportionately impact underserved Black and Hispanic communities. Yet among Black and Hispanic adults, nearly 80% report never having a doctor or healthcare provider discuss PAD with them, which vascular experts say is a major problem.
For this reason, four leading heart and vascular societies recently partnered to create the PAD Pulse Alliance to raise both public and primary care physician awareness about PAD and empower patients to kick off the conversation with their doctor. The partners include the Association of Black Cardiologists (ABC), Society for Cardiovascular Angiography and Interventions (SCAI), Society of Interventional Radiology (SIR) and Society of Vascular Surgery (SVS).
"These new insights are particularly concerning among those most at risk and come at a time when a staggering 1 in 20 Americans over 50 years of age experience PAD," said SCAI President George D. Dangas, MD, PhD, MSCAI in a statement. "The survey confirms what we feared: millions don't have the tools they need to help start a conversation with their healthcare providers because patients are unaware of their risks and the common signs and symptoms. That's why we're encouraging anyone with leading risk factors, diabetes, high blood pressure and use of tobacco products, to know your 'three for PAD' and talk to your doctor."
Inequity in leg amputations and PAD prevalence in Blacks and Hispanics
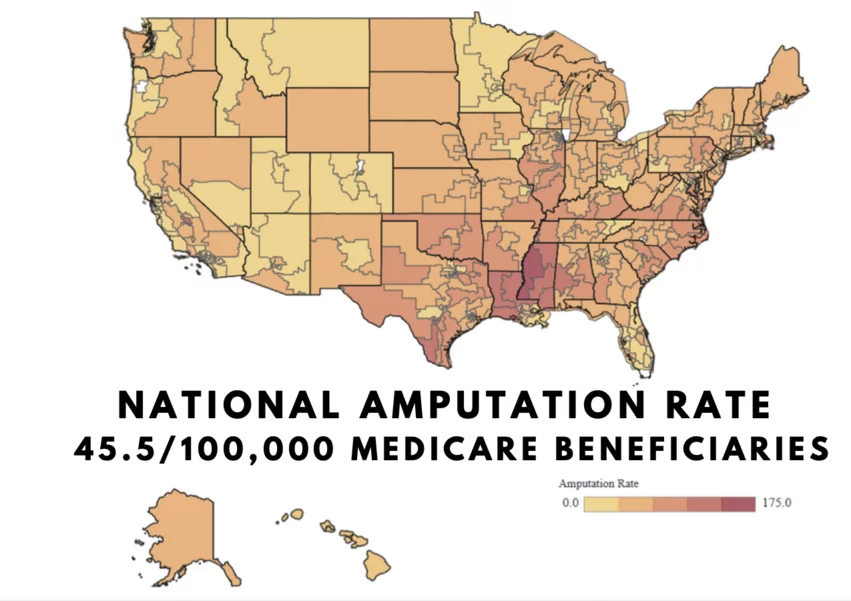
Black people are twice as likely to suffer from PAD and its end-stage condition of critical limb ischemia (CLI), making them and up to four times more likely to undergo an amputation compared than white people. Hispanics present with more progressive PAD, leading to worse outcomes and an even greater risk of amputation.
"The disturbing variations in PAD prevalence, treatments and outcomes underscore another perilous consequence of the health equity gap in managing chronic conditions," Foluso Fakorede, MD, CEO of Cardiovascular Solutions of Central Mississippi and co-chair of the ABC PAD Initiative, said in a statement from SCAI. "It's critical to increase awareness among racial and ethnically marginalized communities and the providers who serve them to close the gap. This campaign is one way we are doing just that, but it will take an ongoing conversation to ensure we're meeting patients where they are with the tools and resources they need."
Fakorede, passionate about the issue of PAD and the inequity of leg amputations, decided to do something about it by opening a cardiology practice in Cleveland, Mississippi, in the epicenter of PAD and amputations in the rural South. For his work on PAD and community engagement, he was given awards by the National Medical Association and the American Heart Association. His work has led to a decrease of 88% in patient amputation rates in his area.
"I think a lot of the work has been seeking out partnerships with community and societal partnerships to see how we can best address this in other communities that look like ours. And not just the Black community, it's the Hispanic community, is the Native American communities, communities that actually have higher disproportional rates of peripheral cure disease. And it is a campaign like this where we are having four big societies actually coming together to talk about PAD awareness and how we can do better," Fakorede told Cardiovascular Business.
This epidemic PAD and amputations is not just in rural areas, but also in many major cities with lower-income Black and Hispanic neighborhoods such as Chicago. Kumar Madassery, MD, director of Peripheral Vascular Intervention and the CLI Program at Rush University Medical Center in Chicago, said he sees a high percentage of severe PAD and CLI patients from the south and west sides of the city coming to Rush for treatment because they are heavily debilitated or have non-healing diabetic foot ulcers.
"Unfortunately a lot of the patients I am seeing have wounds on their foot that are not healing because they do not have enough blood flow and their diabetes is out of control, and unfortunately a large proportion of these patients in this country get a major amputation. In these patients, that carries the highest mortality rate compared to most cancers, above 55%. S that is more than most of the cancers people are aware of, but from a global and a national stance, we have not done a good job of educating patients from how to avoid ever getting into this situation. While I love that I can work with surgeons and save a leg, we need to get better at working together to make sure a patient never gets into this disease spectrum or the later stages of PAD," Madassery told Cardiovascular Business in an interview.
Risk factors and symptoms of PAD
The top three risk factors for PAD are diabetes, high blood pressure and the use of tobacco products. People with diabetes are three to four times more likely to suffer from PAD, while 35 to 55% of people with PAD also have high blood pressure. Alarmingly, 80% of patients with PAD are smokers or former smokers.
Nearly 75% of Black and Hispanic adults surveyed report having or knowing someone who has diabetes, high blood pressure, or is a smoker, but only 30% believe they could be at risk. This is in stark contrast to real-world impact PAD and CLI is having in their communities.
Often, signs and symptoms of PAD can go unrecognized or are easily dismissed. Leg pain that occurs while walking and stops with rest is one of the first symptoms of PAD. However, nearly all survey respondents (91%) say they would dismiss pain as just part of getting older.
"Screening for PAD is easy, quick, and noninvasive. Yet, this survey confirmed that critical patient-provider conversations addressing common symptoms aren't happening," said SIR President Alda L. Tam, MD, MBA, an interventional radiologist and professor in the department of interventional radiology at the University of Texas MD Anderson Cancer Center, in a statement. "If we can educate more people on the risk factors and early warning signs associated with PAD, it's our hope we can foster dialogue earlier between providers and patients to kick off screening and treatment – ultimately preventing amputations and saving lives."
The PAD Pulse Alliance published a website and patient toolkit, available at PADPulse.org.