FFR-angiography guided lesion selection for PCI improves two-year outcomes in TCT late-breaker
New data from the FAVOR III China Trial found that Quantitative Flow Ratio (QFR) guided lesion selection for percutaneous coronary intervention (PCI) improved two-year clinical outcomes, compared with standard of angiography guidance. The benefits were most pronounced among patients in whom QFR assessment altered the planned revascularization strategy.
The findings were reported at the 2022 Transcatheter Cardiovascular Therapeutics (TCT) annual scientific symposium. The results from the FAVOR III China Trial were also simultaneously published in the Journal of the American College of Cardiology (JACC).[1]
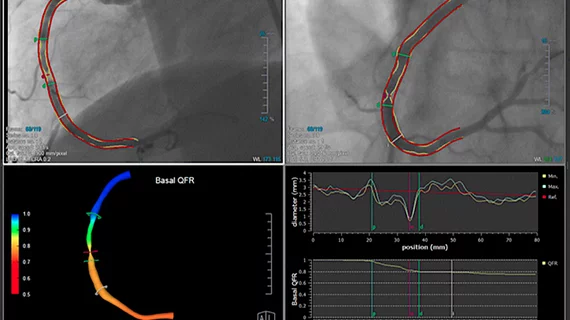
QFR is a product of Medis Medical Imaging, which uses a sweep of the C-arm around the patient in the cath lab to create a 3-D rendering of the vessel segment and a color coded map showing physiological information on blood flow within that vessel. It is an angiography derived fractional flow reserve (FFR) assessment of of hemodynamics, which can help pin point which lesions are the cause of ischemia.
QFR enables online estimation of fractional flow reserve (FFR) without the use of a pressure wire or pharmacologic agents to induce hyperemia.
“Two-year outcomes of a QFR-guided vessel and lesion selection strategy showed that the benefits of QFR guidance continued to accrue over time compared with standard angiography guidance in patients undergoing PCI,” said Lei Song, MD, professor of interventional cardiology, Fuwai Hospital, National Center for Cardiovascular Disease, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China, said in a statement from the Cardiovascular Research Foundation (CRF). “Improvement was greatest among patients in whom the PCI strategy was modified by QFR as well as those who had QFR-concordant PCI. Longer-term follow-up is needed to determine whether the 2-year benefits of QFR guidance for PCI lesion selection are preserved, increase or diminish over time.”
Details of the FAVOR III China Trial using QFR
Overall, the trial found use of QFR resulted in PCI being performed less frequently, fewer stents and less contrast being used. The residual SYNTAX score was also lower in the QFR-guided group compared with the angiography-guided group in those patients who had the PCI strategy changed.
In addition, results were consistent within the first year and between one to two years.
FAVOR III China was an investigator-initiated, multi-center, sham-controlled blinded, randomized trial that compared QFR guidance with standard angiography guidance for lesion selection and monitored outcomes post procedure. The pivotal randomized FAVOR III China demonstrated that lesion selection for PCI using QFR guidance improved one-year clinical outcomes compared with conventional angiographic guidance.
Among the 3,825 randomized participants, two-year major adverse cardiac events (MACE), a composite of all-cause death, myocardial infarction (MI) or ischemia-driven revascularization (IDR), occurred in 8.5% of patients in the QFR-guided group compared to 12.5% of patients in the angiography-guided group (HR 0.66, 95% CI 0.54-0.81, p<0.0001). This was driven by fewer MIs (4% vs. 6.8%, HR 0.58, 95% CI 0.44-0.77, p=0.0002) and IDRs (4.2% vs. 5.8%; HR 0.71, 95% CI 0.53-0.95, p=0.02) in the QFR-guided group.
Compared with the pre-randomization intended lesion selection based on angiography guidance, the revascularization strategy was changed after randomization in 445 (23.3%) patients in the QFR-guided group and 119 (6.2%) in the angiography-guided group (P<0.0001), due to treatment deferral of at least one vessel originally intended for PCI (19.6% vs. 5.2% respectively, P<0.0001) and unplanned PCI of at least one vessel not originally intended to be treated (4.4% vs. 1.5% respectively, P<0.0001).
Although the MACE rate at two years was lower with QFR guidance in both patients in whom the pre-planned PCI revascularization strategy changed (HR 0.34, 95% CI 0.21-0.55) and did not change (HR 0.70, 95% CI 0.56-0.88) after randomization, those with strategy changes had a greater relative reduction in MACE (pint=0.009), driven by better outcomes in patients in whom vessels that had been intended to be treated were deferred after QFR assessment. Patients with pre-PCI QFR-concordant versus non-concordant treatment had a lower risk of two-year MACE (8.8% vs. 17.2%, P<0.0001) and MACE excluding PMI (6.1% vs. 11.9%, P<0.0001).
The benefit of QFR-concordant treatment was present in both patients randomized to QFR guidance and angiography guidance.
The study received grant support from the National Clinical Research Center for Cardiovascular Diseases, Fuwai Hospital (Grant No. NCRC2020001), Beijing Municipal Science and Technology Commission (Grant No. Z191100006619107), and National High Level Hospital Clinical Research Funding (Grant Number: 2022-GSP-GG-20). Pulse Medical (Shanghai, China) provided the QFR system and software at no charge for the study.