FFR-guided PCI provides significant value, new meta-analysis confirms
Using fractional flow reserve (FFR) measurements to guide percutaneous coronary intervention (PCI) procedures for patients presenting with multivessel coronary artery disease (CAD) is associated with fewer stent implantations, according to a new meta-analysis published in the American Journal of Cardiology.[1] The study’s authors also emphasized that FFR-guided PCI can help improve resource utilization by identifying lesions that do not require treatment.
After reviewing multiple databases and making exclusions when necessary, the group landed on three randomized controlled trials (RCTs) for its meta-analysis. Those RCTs include nearly 3,100 PCI patients with an average age of 64 years old. Eighty percent of patients were male. While 23% of patients presented with diabetes, 55% presented with hypertension, 57% presented with dyslipidemia, 31% were current smokers and another 20% had a history of myocardial infarction (MI). The RCTs all compared FFR-guided PCI with angiography-guided PCI among patients with multivessel CAD.
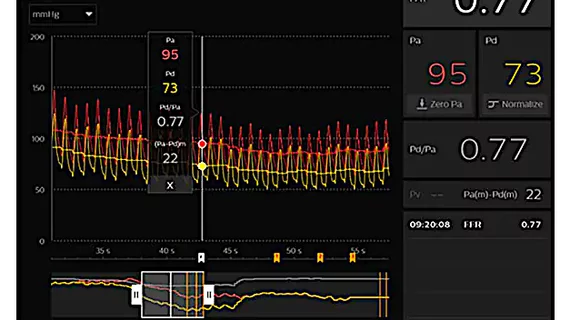
Overall, 59% of lesions that underwent a FFR measurement had an FFR value of 0.80 or less; this is generally believed to be the cut-off for a clinically significant FFR. The average number of stents used during an FFR-guided procedure was found to be “significantly lower” than the average used during angiography-guided procedures.
“Our findings show that with an FFR-guided PCI strategy in patients with multivessel CAD, 40% of lesions that are classified as angiographically significant can be reclassified as not physiologically significant,” wrote first author Connor Jack Matthews, MBChB, BSc, of Leeds General Infirmary in the U.K., and colleagues.
The study’s composite endpoint was death, nonfatal MI or repeat revascularization after one year. This was seen in 10.7% of FFR-guided PCI patients and 11.8% of angiography-guided PCI patients, a small enough difference that it was not found to be clinically significant. The one-year rates of all-cause mortality, nonfatal MI and repeat revascularization were all also comparable when observing each one separately.
The team did note that their work had certain limitations. Follow-up was limited to just one year, for example, and researchers were unable to carry out a more in-depth, patient-level analysis due to the way they designed their study.
Matthews et al. concluded that FFR-guided PCI is a “helpful” resource that could make a considerable impact on patient care.
“Up to 40% of angiographically significant lesions can be safely deferred; this would reduce procedure times, contrast agent dose, and radiation dose for patients and would improve resource utilization in clinical practice,” they wrote.