Impella use may not improve high-risk PCI outcomes
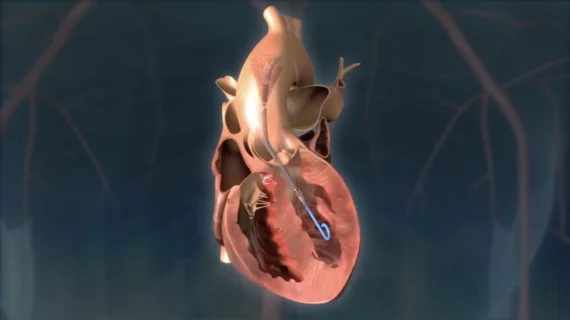
Using Abiomed’s Impella heart pumps to support patients undergoing high-risk percutaneous coronary intervention (HR-PCI) may not provide as much value as initial research suggested, according to a new analysis published in The American Journal of Cardiology.[1]
“HR-PCI has become increasingly common with the advancement of PCI techniques, equipment, and dedicated training,” wrote corresponding author Ron Waksman, MD, director of cardiology at the MedStar Heart Institute and a professor of medicine at Georgetown University, and colleagues. “It is plausible that elevated risk of adverse events associated with interventions may be mitigated by mechanical circulatory support (MCS) with Impella, by avoiding intraprocedural ischemia and consequent hypotension that lead to acute kidney injury (AKI), neurologic dysfunction, or cardiac arrest. However, the PROTECT II randomized controlled trial and observational data demonstrated equivocal results regarding the benefit of protected versus unprotected HR-PCI. PROTECT III registry data indicated a benefit of using Impella CP in contemporary patients who undergo HR-PCI when compared with a historical cohort. However, these data have not been compared directly with a cohort without Impella use.”
To learn more, Waksman et al. compared PROTECT III registry data from 504 high-risk PCI patients treated with an Impella CP device with retrospective data from another 200 high-risk PCI patients treated without Impella support from 2003 to 2018. Among those patients who were not treated with an Impella, 179 received no MCS at all and the other 21 were treated with an intra-aortic balloon pump (IABP). All patients from all groups were 18 years or older.
The non-Impella patients tended to be older—their mean age was 73.4 years old vs. 69.3 years old for Impella patients—and were more likely to present with hypertension or prior coronary artery bypass grafting. Mean left ventricular ejection fraction was also higher among non-Impella patients (23.8%) than Impella patients (22.6%).
Overall, in-hospital major adverse cardiac events (MACEs) were seen in 4.8% of Impella patients and 3% of non-Impella patients. The MACE rates after 90 days, meanwhile, were 13.8% for Impella patients and 7.5% for non-Impella patients. This difference in 90-day incomes was primary driven by fewer deaths in the Non-Impella group.
Impella patients, the authors added, were associated with a significantly lower rate of in-hospital AKI—5.4% vs. 10.5%, to be exact—than non-Impella patients.
“The purported benefit of Impella in HR-PCI is to enable safe intervention in patients with less cardiac reserve while also facilitating high-quality, durable PCI,” Waksman et al. wrote. “However, current clinical evidence does not consistently support the efficacy of Impella in the patient with nonemergent HR-PCI.”
The group noted that their research may lead to speculation that the Impella patients presented with much more complex lesions. However, they wrote, the large number of type B and type C lesions in the non-Impella group and the similar chronic total occlusion intervention rates between the two groups suggest this is not the case.
When it comes to patient safety, the authors found that using Impella was not associated with a heightened risk of bleeding or vascular complications. Prior research had suggested this may be an issue worth keeping a close eye on.
The authors also called for more long-term studies into the potential benefits of Impella use when treating high-risk PCI patients. This could help determine if Impella devices help facilitate complete revascularization.
“Although this study did not find a benefit of Impella use in HR-PCI, this effect may be due to difficulty in determining which patients are truly at great risk and more likely to benefit from Impella usage,” the team wrote. “Of note, a recent trial found that Impella use, compared with no MCS, reduced mortality in patients with cardiogenic shock who underwent PCI for ST-elevation MI, and the benefit was more pronounced in the subgroup of patients with significant hypotension. The definition of elective, stable HR-PCI is, however, vague and not universally agreed on.”
Click here for the full study.