Intravascular lithotripsy, the technology at heart of $13B acquisition, linked to positive real-world data
Intravascular lithotripsy (IVL) technology is gaining popularity among interventional cardiologists, according to new research published in JACC: Cardiovascular Interventions.[1] In addition, coronary IVL is consistently associated with percutaneous coronary intervention (PCI) outcomes comparable to coronary atherectomy.
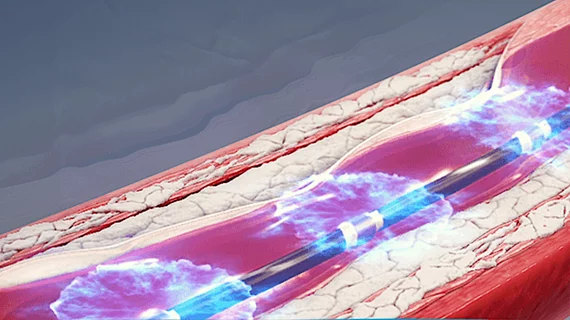
IVL targets severely calcified plaques in the coronary and peripheral arteries with shockwaves, clearing the way for cardiologists before PCI. The technology’s rapid rise among U.S. providers after it received U.S. Food and Drug Administration (FDA) approval has been one of the industry’s biggest success stories in recent years. Shockwave Medical, the company that originally developed IVL, was acquired by Johnson & Johnson for approximately $13.1 billion in early 2024 after stringing together several clinical and policy victories.
But how does IVL compared to other treatment options? That is exactly what the team behind this new analysis hoped to learn.
“Since the introduction of IVL to the U.S. PCI market in 2021, few large-scale evaluations have been performed to evaluate the uptake and outcomes of this novel technology in real-world practice,” wrote first author Hitinder S. Gurm, MBBS, an interventional cardiologist with the University of Michigan Health System, and colleagues. “Therefore, we investigated contemporary trends and outcomes associated with coronary IVL among patients who underwent PCI in the state of Michigan and reported coronary atherectomy trends and outcomes as a comparator.”
Gurm et al. tracked data from more than 42,000 PCI patients treated at one of 48 Michigan facilities from January 2021 to June 2022. While IVL alone was used on 2.6% of patients, atherectomy alone was used on 4.1% and the two treatments were used together on 0.6%. IVL use increased as time went on, with care teams using it for just 0.04% of PCIs in January 2021 and 4.3% by June 2022. (Atherectomy use, meanwhile, decreased during the same time.)
“This early adoption of IVL may be related to the ease of use of this device given that every interventional cardiologist is familiar with delivering and inflating an angioplasty balloon,” the authors wrote.
Patients treated with IVL and atherectomy presented with comparable clinical and demographic characteristics, and the most commonly treated target for both groups was the left anterior descending coronary artery. The group did note that prior PCI was more likely in patients who were ultimately treated with IVL. IVL patients were also more likely to have a prior myocardial infarction—this is one subset of patients, the authors noted, that was often not included in clinical trials focused on IVL.
Diving into patient outcomes, Gurm and colleagues found that the overall major adverse cardiovascular event (MACE) rates were similar for the two treatment options. Perforation was the one adverse event where there was a significant difference, where it was significantly more likely among patients treated with atherectomy.
Procedural success rates were also similar, surely a welcoming sign to all interventional cardiologists.
“Since its FDA approval in February 2021, IVL use has increased dramatically and is now the most common calcium modification device used in contemporary practice,” the authors concluded. “IVL and atherectomy use are associated with similar and generally low rates of complications and high rates of procedural success among all-comers and within important patient subgroups. These devices are frequently used in patients who would not have met the criteria for enrollment in the pivotal clinical trials; thus, continued postmarket surveillance to ensure the safe use of these devices is warranted.”
Click here to read the full study in JACC: Cardiovascular Interventions, an American College of Cardiology journal.