Pulmonary artery denervation shows promise to treat pulmonary arterial hypertension
A late-breaking sham-controlled clinical evaluation of pulmonary artery denervation (PADN) for patients with pulmonary arterial hypertension (PAH) found that in addition to increasing exercise capacity, PADN improved hemodynamics and clinical outcomes during six-month follow-up.
Findings were presented as a late-breaking study the Transcatheter Cardiovascular Therapeutics (TCT) 2022 meeting. This trial caused buzz from several key interventional cardiology opinion leaders, who felt this was a major step forward in being able to address this difficult-to-treat patient population.
“This study clearly demonstrates that treatment with PADN plus a PDE-5i was safe and resulted in improved exercise capacity at six months compared with PDE-5i treatment alone,” Shao-Liang Chen, MD, PhD, director of cardiology and cath lab, Nanjing First Hospital, said in a statement from the Cardiovascular Research Foundation (CRF). Chen is also vice president of Nanjing First Hospital, Nanjing Medical University and professor of internal medicine and cardiology, Nanjing Medical University. “In addition, we found significant improvements in hemodynamics as well as a reduction in clinical worsening with PADN. Larger randomized trials are needed to demonstrate the incremental benefits of PADN in patients on combination pharmacotherapy.”
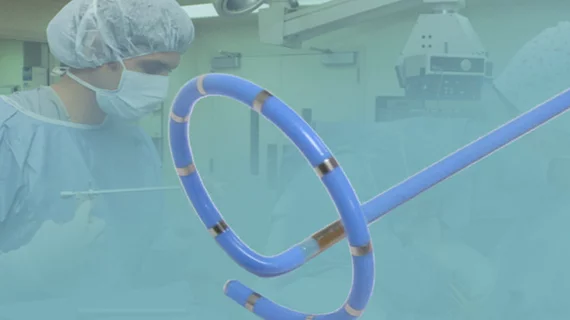
The trial used a dedicated radiofrequency ablation pulmonary artery denervation catheter produced by Chinese medical technology company Pulnovo. In February 2021, the devices was granted the U.S. Food and Drug Administration (FDA) breakthrough device designation
PAH is a progressive, debilitating disease characterized by obliterative pulmonary vascular remodeling with elevated pulmonary vascular resistance. Despite advances in medical treatment, PAH is associated with a poor long-term prognosis. Previous observational studies have demonstrated that PADN improves hemodynamic and exercise capacity in patients with PAH, but the technology had not yet been studied in a randomized trial until this study.
Details on the pulmonary artery denervation trial
Between January 2018 and June 2021, 128 PAH patients were randomized to PADN (n=63) or a sham procedure (n=65) at 11 centers in China. Patients not taking PAH-specific drugs for at least 30 days were enrolled. Both PADN and sham procedure patients received a phosphodiesterase-5 inhibitor (PDE-5i).
For the sham procedure, the PADN catheter was positioned at the target site, but ablation was not performed.
Measurement of N-terminal-pro brain natriuretic peptide (NT-proBNP), a six-minute walk test (6MWD), and transthoracic echocardiography were performed at baseline and at days 7, 30 and 180 using standardized procedures.
The primary endpoint was the between-group difference in the change in 6MWD from baseline to six months. The 6MWD improved in both groups during follow-up, with the between-group difference becoming significant by 30 days. The median change from baseline to six months was 61.0 m (12 to 92) in the PADN group and 18 m (-9 to 66) in the sham group (p=0.004). The adjusted between-group mean difference in the change of 6MWD from baseline to six months was 33.8 m (95% CI, 16.7 to 50.9; p<0.001).
At six months, PVR was reduced by -3 ± 0.3 Wood units after PADN and -1.9 ± 0.3 Wood units after sham (adjusted difference -1.4, 95% CI -2.6 to -0.2). PADN also improved right ventricular function, reduced tricuspid regurgitation and decreased NT-proBNP. Clinical worsening was also less (1.6% vs. 13.8%; OR 0.11, 95% CI 0.01 to 0.87) and a satisfactory clinical response was greater (57.1% vs. 32.3%; OR 2.79, 95% CI 1.37 to 5.82) with PADN treatment.
The study was supported by the National Scientific Foundation of China (grant number NSFC 91639303, NSFC 81770441 and NSFC 82121001). Nanjing First Hospital funded the trial and Pulnovo provided all PADN catheters through the study period.
Disclosures: Chen reported being the inventor of PADN, but not the owner of the PADN patent. He receives speaker honoraria from Pulnovo and grants from the National Scientific Foundation of China.