Q&A: Ken Rosenfield explains the impact of new reimbursement coverage for carotid stenting
The Centers for Medicare and Medicaid Services (CMS) changed its national coverage determination (NCD) for carotid artery stenting (CAS) procedures to greatly broaden the number of patients eligible for reimbursement. This will make it much easier for patients to receive the minimally invasive procedure as an alternative to open surgical carotid endarterectomy (CEA). It is also expected to be a boost in revenue for interventional labs performing this procedure as volumes start to increase.
CMS made the change based on a 2022 formal request for review from the Multispecialty Carotid Alliance (MSCA), a group of key opinion leaders in interventional cardiology, neurology and vascular surgery. CMS announced its new coverage determination for CAS on Oct. 10, 2023.
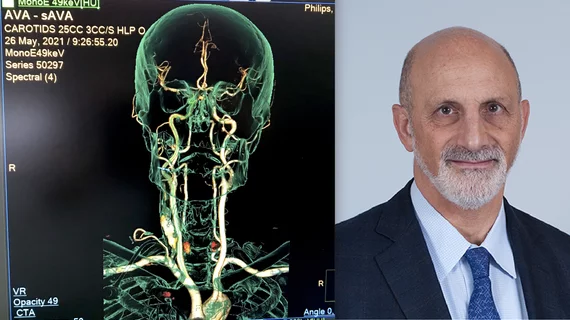
The point person for the MSCA is Ken Rosenfield, MD, section head of vascular medicine and intervention at Massachusetts General Hospital. He shared his thoughts on the new CMS policy for CAS with Cardiovascular Business and outlined its expected impact.
Cardiovascular Business: How will this update impact patient access to these procedures?
Ken Rosenfield: We will undoubtedly see a significant increase in the use of stenting in general, and especially transfemoral (TF) and transradial (TR) CAS. Many patients prefer these approaches, which are less invasive and, based on an overwhelming body of evidence, equally as effective and safe as CEA and transcarotid artery revascularization (TCAR). My guess is that CEA and TCAR will continue to have important roles, but many patients will opt for TF or TR stenting over CEA and even TCAR.
CMS has mandated that patients be fully informed of their options, and that a shared decision-making process be undertaken for all carotid revascularization procedures. This is meaningful, as many have either not been fully informed of their options, or CAS was not an option.
The rise in volume of CAS will be gradual, as we need to increase awareness among patients and referring providers. Also, importantly, we must train additional interventionalists and surgeons about proper case selection and safe techniques. The MSCA is now a 501c6 NFP organization that is committed to optimizing CAS outcomes through education, training and quality assurance.
What impact will this change in reimbursement coverage likely have on vascular and cardiology cath labs?
Cath labs and interventional programs will need to gear up, both in terms of training physicians and staff, and ensuring that inventories are complete. As a vascular community, we must act responsibly, establish standards and encourage peer review and quality assurance.
Why has it taken so long for CMS to expand coverage in light of all the clinical evidence that has been gathered over the past 14 years?
You are correct that the evidence collected demonstrating comparable outcomes is overwhelming, more than for just about any other procedure or therapy in the vascular space. Access for patients to CAS has been a long time coming. CMS was appropriately waiting for the publication of level I evidence from well-constructed comparative effectiveness trials in respected peer-reviewed journals. That occurred several years ago with the publication of CREST I and ACT I in NEJM.[1,2]
Despite all the evidence, there has been controversy about the role of CAS, as medical therapy has improved and other therapies like TCAR were developed. Everyone in this space is aware of the politics of CAS, one only needs to look at the comments to CMS. Over 750 comments were submitted, and the 50% that were opposed came predominantly from vascular surgeons. There were 14 medical organizations, including all of the neurology, neurosurgery, radiology, cardiology, and vascular medicine societies, as well as American Heart Association (AHA), commenting in favor of covering CAS. Sadly, there was one entity, the Society for Vascular Surgery (SVS) that was opposed.
CMS did a beautiful job of cutting through the political noise and making a decision that is right for patients. Vascular surgeons play a central role in managing patients with carotid disease and MSCA believes many will retrain and embrace CAS as an excellent treatment, especially as the technology advances to improve outcomes.
Is carotid stenting less expensive than carotid endarterectomy? What is the difference is costs for the procedures or in the downstream costs for the patient in terms of recovery, etc.?
The small number of studies comparing the cost of CEA to CAS have generally shown similar costs, as the cost of the OR is offset by that of the devices. The cost of TCAR, at least in one study, was considerably higher than either CAS or CES. This is not unexpected, since the devices (stent and protection systems) are added to the costs of the OR and the anesthesiologist. Recovery costs vary depending upon patient substrate, but are likely not that different at present. More data will be required to truly assess the relative cost of each of these approaches.
Overall, what are your feelings about this change in CMS policy?
The carotid NCD is great news for patients. Medicare patients, and presumably patients covered by other payers, will now have access to the full range of revascularization options for reductions in stroke risk, including CAS, TCAR and CEA. Interestingly, in their decision, the Coverage Analysis Group of CMS basically said that stenting is a good therapy for carotid stenosis, regardless of how that stent is delivered (whether by femoral, radial, or trans-carotid approach). CMS also emphasized that the use of CAS and CEA should be reserved for only those carefully selected patients in whom revascularization on top of optimal medical therapy is deemed appropriate.
The ongoing CREST 2 study will help us understand which patients are appropriate. That said, it is my belief that technological advances over the next five to seven years will continue to improve the technique and its outcomes, and enable us to consistently achieve stroke and death rates well under 1%.