Targeting coronary inflammation helps cardiologists provide better care
In recent years, there has been a growing interest in the role of inflammation in coronary disease development, leading to groundbreaking research and the 2023 U.S. Food and Drug Administration (FDA) approval of colchicine (Lodoco) as the first drug to treat coronary inflammation. Since then, cardiologists have been looking for additional information on how to detect and manage this previously ignored cause of heart disease.
"For years now, we've been able to target the lipids and blood pressure. But cardiologists, we really haven't had much in the way of targeting inflammation. That's really what's so exciting ... we finally have medications that are being tested and also approved for targeting inflammation to reduce cardiovascular risk," explained Michael Garshick, MD, director of the cardio-rheumatology program, cardiologist, and assistant professor at the Ronald O. Perelman Department of Dermatology with NYU Grossman School of Medicine. He spoke with Cardiovascular Business on the significance of inflammation in cardiovascular health and the strides made in preventive cardiac care.
Inflammation has not been a big area of study and treatment by cardiologists, despite some inflammatory response in arteries being a primary reason why some atherosclerotic plaques become unstable vulnerable plaque prone to rupture and resulting in heart attacks. Without inflammation, the plaques remain stable. But attention to inflammation is now changing.
"Cardiologists are actually a bit behind in the field of inflammation compared to oncologists, immunologists, rheumatologists, dermatologists, even the gastroenterologists who are now involved with inflammatory bowel disease," Garshick explained.
Coronary inflammation research
Garshick has been researching inflammation's connection to coronary disease for the past nine years. He said the pivotal Cantos clinical trial, which targeted the inflammasome IL-1 beta to IL-6 CRP pathway, demonstrating a reduction in cardiovascular events by specifically addressing inflammation.[1] This marked a shift in cardiology thinking, encouraging exploration beyond traditional risk factors like lipids and blood pressure.
At NYU, Garshick uses psoriasis, a skin condition, as a model to study how inflammation contributes to atherothrombosis. Psoriasis has been linked to an elevated risk of cardiovascular disease, showcasing the intricate connection between systemic inflammation and heart health.
"The IL-1 beta to IL-6 CRP pathway was actually the highest differentiated express pathway in psoriasis. And so that really solidified in my mind how we can use a skin condition such as psoriasis as a translational overlap with nonspecific inflammation such as inflammasome processes and how it may promote cardiovascular disease. I think that's how my own evolution in this field has evolved and how what we've done an NYU has helped contribute to this field by showing how this inflammasome pathway can be implicated in autoimmune disease and how it relates to cardiovascular risk as well," Garshick said.
This research has placed him in the unique position as a cardiologist working in the NYU department of dermatology. Several other academic hospitals are researching this translational inflammation link between psoriasis and coronary disease, which has led to a number of cardiology/dermatology collaborations.
Unaddressed coronary inflammation leads to residual risk of heart attacks
While some cardiac patients are managed well for lipids and blood pressure, some still have heart attacks and many experts are saying this is because the inflammation is not being addressed. This has led to the concept of the residual risk due to inflammation.
Garshick said there have been studies attempting to address the residual risk by reversing vascular inflammation induced by psoriasis. But these studies, while largely negative, emphasize the persistent challenge of managing underlying systemic inflammation even after targeting specific conditions.
Residual inflammatory risk in contemporary statin-treated patients was one of the late-breaking studies presented at the ACC.23. Paul M. Ridker, MD, director of the Center for Cardiovascular Disease Prevention and a professor at Brigham and Women's Hospital, presented the results and spoke with Cardiovascular Business in this interview.
FDA clears first drug to treat coronary inflammation
The FDA approval of the anti-inflammatory medication colchicine is viewed by many experts in cardiology as a way to improve preventive cardiac care. Colchicine has been used for decades in the treatment of gout and for various dermatological indications, including psoriasis. Some cardiology experts in coronary inflammation had been advocating for years for off-label use of the drug in high-risk patients to reduce the residual risk. With the FDA clearance of Lodoco, cardiologists have become much more open to the idea, as seen in packed sessions on this topic at cardiology meetings.
Garshick notes the controversy surrounding the drug's interactions, affordability, access and dosage. For these reasons, he said it is important to identify the right patients who may benefit from colchicine, especially those with elevated C-reactive protein (CRP) levels. In addition to blood tests, he said new imaging techniques to better visualize coronary inflammation are also being developed.
"I think the first step is identifying those patients who could be candidates for it, whether that's with an elevated CRP or not, or just someone who you don't quite understand why they've had such aggressive atherosclerosis despite the lipids not being that high or well controlled, or despite not being obese or family history, etc. You do have something else to offer these patients now that is relatively safe and it is not an aggressive," Garshick explained
He stressed the safety and of the drug in patients with normal kidney function.
"According to the clinical trials, it is generally a very safe medication, as long as you have the right monitoring parameters in place," Garshick added.
Cardiologists do not widely use C-reactive protein testing for inflammation
While CRP testing has been available for years, it is not widely used in cardiology for measuring levels of coronary inflammation. However, Garshick anticipates a gradual shift in its routine use.
"It is very, very underutilized. I think it's not in the standard order set for many cardiologists the way we think about lipids or hemoglobin A1C, even lipoprotein little A to some extent. I think it is happening, it is just slow," he said.
At NYU, he said adoption of CRP is increasing, some preventive cardiologists ordering it on many patients. He said it helps that NYU is involved in anti-inflammatory clinical trials, which raise awareness, but some of the cardiologists are still having trouble getting CRPs routinely drawn.
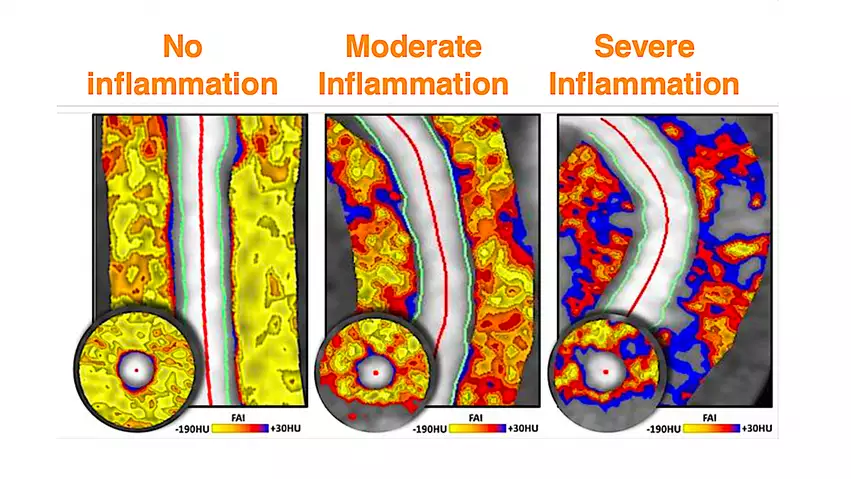
Fat attenuation index (FAI) CT imaging of the fat surrounding coronary arteries can show inflammation in the vessel wall and help pin-point vulnerable plaques. This also can show the reversal of inflammation due to drug therapies. The technology is being developed by the vendor Caristo, which has European CE mark and the company is seeking FDA clearance.
Detecting and monitoring coronary inflammation via imaging
While CRP will show elevated inflammation in the body, new medical imaging techniques are able to directly show inflammation in the walls of coronary arteries. Garshick emphasizes the need for improved biomarkers to more specifically detect the impact of inflammation in vessels that can lead to hearts attacks and strokes. He said nuclear imaging and a new coronary computed tomography angiography (CCTA) technology may be able to help in the near future.
"From the imaging perspective, there's adipose tissue that surrounds the coronary vasculature and there's been a lot of talk recently about using imaging techniques to understand how metabolically active that adipose tissue is surrounding the coronary vasculature," Garshick explained.
This was one of the big studies presented at the American Heart Association (AHA) 2023 meeting in November by the University of Oxford. It used Caristo's CaRi-Heart artificial intelligence (AI) assessment software to clearly visualize inflammation in the perivascular fat surrounding arteries using a CT scan. As part of the Oxford Risk Factors And Non-invasive imaging (ORFAN) study, about 40,000 CCTA scans were reviewed by the AI from the U.K.'s National Health Service (NHS) records. It was able to link those older CT scans with health outcomes over the following10 years. Almost half of patients without coronary narrowings were reclassified when coronary inflammation, rather than only plaque alone, was taken into account.
The company is currently in discussions with the FDA and expects to file a de-novo application for regulatory review in early 2024.
Nuclear imaging can also detect areas of inflammation in the body, but Garshick said better radiotracers are needed to look for macrophage uptake specifically in the walls of blood vessels.
"Glucose uptake in the aortic vasculature is not the appropriate metric of overall cardiovascular risk. So we certainly need better radiotracers, newer imaging techniques to look at the coronary vasculature, and better techniques to detect vulnerable plaque in the coronary vasculature. I think these are all in development and coming down the line," he said.
Opening the door to personalized cardiology prevention
Garshick envisions a personalized approach to cardiac prevention, emphasizing the need to understand specific drivers of atherosclerotic risk for individual patients. He predicts a balance between polypharmacy and personalized medicine, with a focus on refining preventive strategies based on a deeper understanding of inflammatory contributions to cardiovascular health.