Can intracardiac echo replace TEE during structural heart procedures?
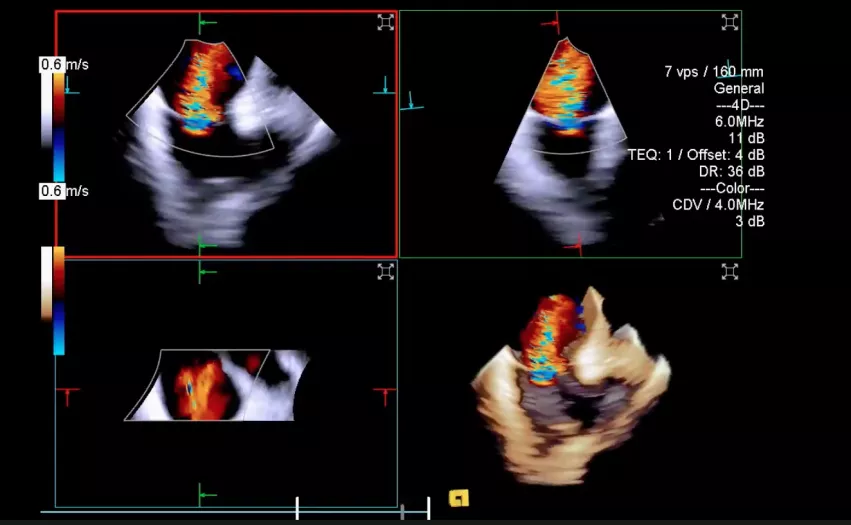
With the introduction of 3D/4D intracardiac echo (ICE) catheters in recent years, there has been growing use of this imaging modality for structural heart periprocedural imaging to simplify procedures and potentially lower costs. Some interventional operators see 3D ICE imaging as good enough to guide transcatheter edge-to-edge repair (TEER) of valves and left atrial appendage occlusions without the need for transesophageal echo (TEE).
TEE has been used to guide most transcatheter structural heart cases over the past decade, but 3D ICE is changing how some centers image these cases. The biggest advantage of ICE is that it can eliminate the need for an anesthesiologist to fully sedate patients so the TEE probe can be inserted down the esophagus. Anesthesiologists add cost to the procedure and an extra body in the procedure room. Using conscious sedation also helps facilitate faster patient recovery. ICE also offers views inside the heart that can sometimes be difficult to image with TEE.
There is the possibility of eliminating the need for an echocardiographer in the procedure, since the interventionist is the person controlling the ICE catheter. However, some centers still believe an interventional echocardiographer is needed because they are an internal part of the heart team and can manipulate the image view on screen and help interpret the image.
At recent cardiology conferences, the role of 3D ICE has been highlighted in atrial appendage occlusion (LAAO) and transcatheter tricuspid valve repairs.
There is growing interest in using 3D ICE for mitral and tricuspid TEER valve procedures, mainly as an adjunct to TEE, Rebecca Hahn, MD, professor of Medicine at Columbia University Irving Medical Center, chief scientific officer of the echo core lab at the Cardiovascular Research Foundation (CRF) and director of interventional echocardiography at the Columbia Structural Heart and Valve Center, told Cardiovascular Business.
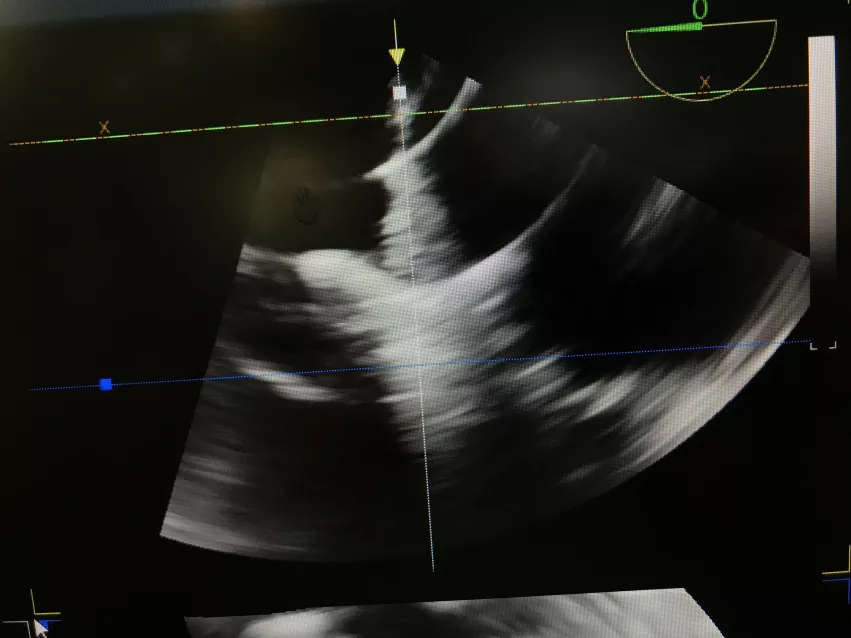
3D ICE offers an additional tool to image transcatheter procedures and overcome issues with suboptimal TEE imaging. TEE has a wider field of view, deeper tissue imaging capability and can obtain views that ICE cannot. For these reasons, 3D ICE is often used in conjunction with TEE in complex procedures. However, some speakers at the Transcatheter Valve Therapies (TVT) structural heart summit said they have moved mainly to ICE only for certain procedures.
"With ICE you don't need the anesthesiologist, you could do an awake case," Hahn said. "At Columbia, depending on the procedure, we are using ICE in conjunction with TEE. In addition, TEE can give you different types of images that ICE has difficulty getting," Hahn explained. "But there are procedures where you might not need TEE."
Using 3D ICE to guide LAA occlusion
Devi Nair, MD, FACC, FHRS, director of cardiac electrophysiology at St. Bernard's Healthcare in Jonesboro, Arkansas, said there is a movement toward using 3D ICE for LAAO in conjunction with or as an alternative to TEE.
"Years ago when we did 2D TEE, we never thought we would get to 3D TEE, and now we are so dependent on 3D TEE. There is something to be said about seeing things in three dimensions. The left atrial appendage is a three-dimensional structure. We are moving away from TEE-guided procedures to ICE-guided procedures, and I think it is important for us to step to the next technology," Nair explained.
However, Nair did said a key barrier to wider ICE adoption is the higher cost of the ICE catheters, in the range of $3,400 per catheter. This is something centers need to consider, as it is possible costs might be offset if ICE can eliminate extra staff or equipment needed during the procedures.
"3D ICE is definitely one step forward, but there are nuances to cost, nuances to acquiring the technology and the need to fine tune the technology, but the future is bright I would say," Nair said.
She also explained how she uses ICE during LAA procedures and the ease of use of the newer systems.
"There are now three 3D/4D ICE catheters that allow us to image the appendage without doing much manipulation. You cannot image the left atrium from the right atrium, so you do need to go into the left atrium with the catheter. But once you are in the left atrium, you don't really have to manipulate the ICE catheter so much," Nair explained.
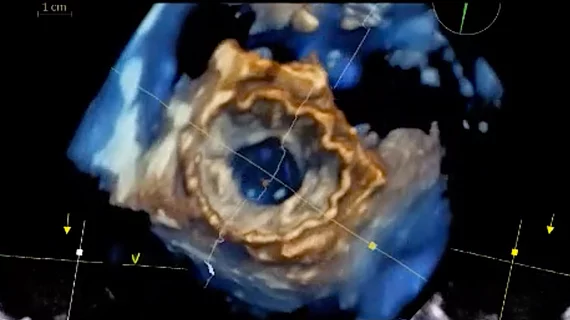
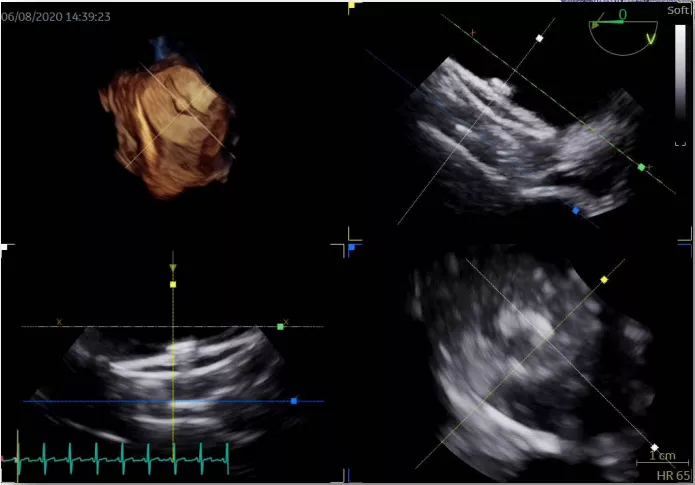
3D ICE allows Nair to get multiplanar renderings (MPR) and do a full volumetric analysis of the appendage and measure the ostium.
"I would not dare to measure the ostium using 2D ICE and size off of that, but 3D is a different story," Nair said.
New generation 3D ICE probes can overcome suboptimal TEE
In recent years, the U.S. Food and Drug Administration (FDA) has cleared three next-generation matrix array intra-cardiac echo probes that enable 3D and 4D imaging. Hahn and Nair said these new technologies have increased interest in 3D ICE in recent years because it better shows the anatomical structures and the relation of devices in live procedural imaging over 2D imaging. These newer ICE probes do offer 2D views and multiplayer reconstruction imaging as well.
"The image quality of these probes is absolutely fantastic," Hahn explained. "It really has changed how we deal with difficult imaging by TEE."
The need for ICE arises for a variety of reasons, according to Hahn. For example, during one MitraClip case, the patient had a very large hiatal hernia which prevented clinicians from getting good TEE images. They used an ICE probe concomitantly with the TEE to navigate the procedure. Imaging the tricuspid valve can be challenging in some patients with TEE because of the need to image through the right side of the heart, and ICE can offer another approach to seeing the anatomy.
The ICE system Columbia is using has the same functionality as their TEE probes, so it is easier for interventional imagers to switch between the two modalities.
Is CT still needed in structural heart procedures?
The question if computed tomography (CT) pre-procedural imaging is needed when a center is using high-quality 3D TEE comes up for discussion frequently in few sessions at the TVT and the Transcatheter Catheter Therapeutics (TCT) meeting.
CT has been a standard in structural heart workups to determine the precise size and shape of the anatomy for device sizing and catheter navigation. CT also shows the relation of neighboring anatomical structures to avoid issues, such as the location of coronary arteries, left ventricular outflow tract cause issues, assessment for device access routes and landing zones for optimal transeptal punctures to ensure proper crossing catheter angles to reach the target anatomy.
The lack of reimbursement for CT planning workups plays a role in some operators or centers opting out of CT use.
For LAAO procedures, which at some centers have become routine, some operators feel they have all the information they need just using 3D TEE or 3D ICE without the need for CT. According to Nair, who was involved in discussions on this in a session at TVT 2022, CT can help enable to the use of ICE-only procedures.
"There is something to be said about preplanning," Nair said. "If a patient can get a CT scan there are several computation algorithms that make the procedures so simple and it takes the surprise factor away. You walk into the case knowing what anatomy you are going for, knowing the dimensions... You know if a patient has a thrombus, you know the ideal transseptal landing zone you need, and you know which device is a better option. A certain device might fit the anatomy better, so it is the right thing for us to choose this ahead of time for our patients so we can get the most optimal seal."
She said CT scans can help enable use of ICE to guide the procedure, because all the guess work and measurements are taken out of the procedure that would usually require additional periprocedural imaging. The procedure can then be guided using just 3D ICE.
"Even if you still want to use TEE and general anesthesia, CT helps make things more efficient because you already know what device you are going in with and you know exactly where the device needs to go and you have a roadmap," Nair explained.