Mitigating risk: How the depth of device implantation impacts LAAO outcomes
Deeper device implantation during left atrial appendage occlusion (LAAO) procedures increases the patient’s risk of developing a blood clot, according to new research published in JACC: Cardiovascular Interventions.[1]
“Growing evidence supports LAAO for stroke prevention in selected patients with nonvalvular atrial fibrillation (AFib),” wrote first author Pedro Cepas-Guillén, MD, PhD, an interventional cardiology fellow with Hospital Clinic de Barcelona in Spain, and colleagues. “Ongoing refinement of the implantation procedure has improved the safety and efficacy of the technique. Nonetheless, device-related thrombus (DRT) remains one of the main concerns because of the increased risk for thromboembolic events.”
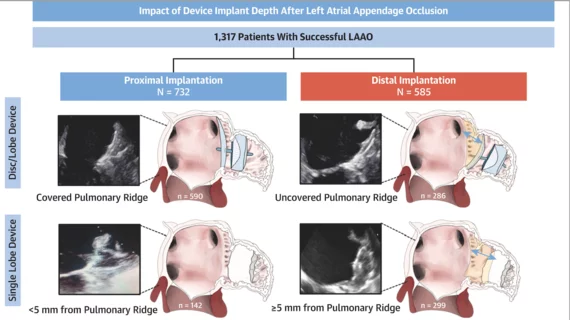
Cepas-Guillén et al. examined data from more than 1,300 patients who underwent a successful LAAO at one of nine facilities in Europe or Canada from 2012 to 2020. The mean patient age was 74.9 years old and more than 64% of patients were men. Decisions related to device type and post-LAAO antithrombotic therapy were made by each care team with no guidance from the study’s authors.
Patients were separated into two groups according to the depth of device implantation and how it related to the patient’s pulmonary ridge (PR). Definitions varied based on whether the patient was treated with a lobe and disc device or single-lobe device. Patients who received a lobe and disc device were placed in the proximal device implantation group if the disc was at the level of the PR, but patients who received a single-lobe device landed in that group if implantation was <5 mm between the edge of the PR and the device’s proximal surface.
In both groups, meanwhile, patients were simply placed in the distal implantation group if they did not meet the criteria for proximal implantation.
Examining data from each procedure, the authors determined that 56% of patients belonged in the proximal implant group and the remaining 44% belonged in the distal implantation group. Patients with permanent nonvalvular AFib and/or chronic heart failure were more likely to be in the distal implantation group than the proximal implantation group. These patients were also more likely to be prescribed direct oral anticoagulants.
Procedural outcomes were not significantly different between the two groups. The combined rate of procedural major adverse events was 5.3% and there were a total of four patient deaths. After a median follow-up period of 21 months, the overall ischemic stroke and major bleeding event rates were comparable between the two groups. All-cause mortality and cardiovascular mortality were also similar.
The primary focus of the team’s study, DRTs, were seen in 2.3% of proximal implantation patients and 12.2% of distal implantation patients. The research team identified a “stepwise increase in DRT incidence” as implantation depths increased.
“Of note, when the LAAO device was implanted more than 15 mm from the PR, DRT rates of 21.6% and 18.6% were observed with the single-lobe and disc and lobe devices, respectively, compared with 1.5% and 2.5% in the proximal implantation group,” the authors wrote.
With single-lobe devices, the rise in DRT risk was primarily seen beyond a depth of 5 mm. For the disc and lobe devices, however, the increase “became progressive beyond the first distal millimeters.”
Eighty-two percent of DRTs were detected within 180 days of the LAAO procedure.
Running a series of analyses, the team determined that distal implantation and nonantithrombotic or single antiplatelet therapy after LAAO were independent predictors of the patient experiencing a DRT. LAAO device type and peridevice leak were not found to be independent predictors of DRT.
“To date, this is the first study to specifically evaluate the role of LAAO device implantation depth on DRT occurrence,” the authors concluded. “Our results showed that LAAO device implantation depth affects DRT rates, with a higher incidence with deeper implantation and larger uncovered areas. Given its clinical impact, proximal device implantation should be the optimal target in patients undergoing LAAO.”
Read the full study here.