ICE-guided Watchman procedures linked to safety concerns—is TEE better for LAAO or will things improve?
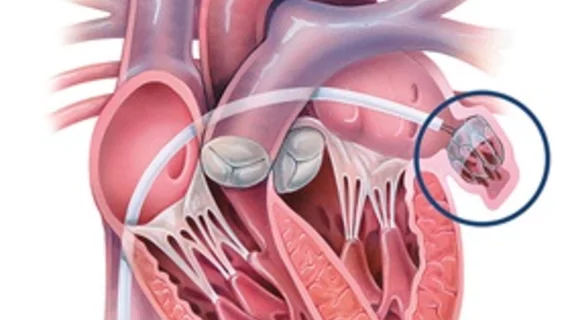
When patients with atrial fibrillation (AFib) require left atrial appendage occlusion (LAAO) to prevent their risk of stroke, the procedures are typically guided by transesophageal echocardiography (TEE). Intracardiac echocardiography (ICE) has emerged as another option for LAAO guidance, but is it really worth considering a switch?
A new analysis in JACC: Clinical Electrophysiology explored that very question.[1] The study’s authors noted that both TEE and ICE have their own advantages and disadvantages.
“TEE is widely available and familiar to most cardiologists, with established protocols that are routinely implemented to obtain high-resolution 3D imaging of intracardiac structures,” wrote corresponding author Jonathan P. Piccini, MD, a professor of medicine and director of the cardiac electrophysiology section at Duke University School of Medicine, and colleagues. “However, TEE exposes patients to the risks of general anesthesia (GA) and esophageal injury. ICE is established in the interventional electrophysiology community owing to advantages like near field imaging, avoidance of GA, lower turnover times and decreased hospital expenses. ICE requires additional vascular access, may require double transeptal puncture and significant intracardiac catheter manipulation, increasing the risk of pericardial injury.”
Piccini et al. examined data from nearly 40,000 patients treated from August 2020 to September 2021 at one of 698 different U.S. facilities. All data came from the American College of Cardiology National Cardiovascular Data Registry LAAO Registry. TEE guidance was used in 80% of cases, and ICE guidance was used in 5.7%. All patients included in this study received a Watchman FLX device from Boston Scientific. Patient were evaluated both at discharge and after 45 days.
Patients treated with the two guidance methods had similar baseline characteristics, including a mean age that was close to 76 years old. Approximately 40% of patients in both groups were women.
From an effectiveness standpoint, the two techniques appeared to be quite similar. Successful implants were seen in 98.3% of ICE patients and 97.6% of TEE patients, for instance, and a complete seal was seen in 95.6% of ICE patients and 95.5% of TEE patients when examined at discharge. The complete steal rates were also similar—83.2% for ICE patients vs. 82.2% for TEE patients—45 days later.
Unadjusted all-cause mortality was higher among ICE patients at discharge, but the difference was no longer statistically significant after 45 days. After making adjustments based on patient characteristics and case volume, however, all-cause mortality was similar for the two methods both at discharge and after 45 days.
The single most noteworthy difference between these two guidance options was the increased risk of pericardial effusion after ICE. For patients evaluated at discharge, the rates of pericardial effusion were 0.9% after ICE and 0.4% after TEE. At 45 days, those rates were 1% for ICE and 0.5% for TEE. The evidence suggests that less experienced operators may have been largely responsible for this discrepancy.
“It is important to highlight that the adjusted rate of pericardial effusion requiring intervention was twice as high in the ICE group compared with TEE,” the authors wrote. “This finding raises concerns especially in light of recent reports from the LAAO Registry with first-generation Watchman devices, where pericardial effusion requiring intervention was associated with a substantially higher risk of major adverse events (including death) both in-hospital and after discharge compared with other periprocedural events like device-related thrombus or peridevice leak. At the same time, it is reassuring that the absolute unadjusted rates of pericardial effusion were overall low in both arms of our study.”
Another key takeaway from the group’s research was that procedural times were slightly shorter for TEE (78 minutes) than ICE (82 minutes). Again, however, this could be because some operators simply have less experience with ICE guidance.
“As operator experience with ICE-guided LAAO increases, further analyses will be less susceptible to confounding as a result of differential operator experience,” the group wrote.
Reviewing their findings, Piccini and colleagues concluded that the concomitant use of ICE and TEE is recommended as operators continue to grow more comfortable with performing ICE-guided LAAO procedures. Seeking out additional training or working with more experienced colleagues “may also help to minimize the risk of complications.”
Co-authors on this analysis included representatives from Beth Israel Deaconess Medical Center, Mayo Clinic, Cleveland Clinic, St Bernard's Heart and Vascular Center, Yale University School of Medicine, Scripps Clinic and the University of California. Two other co-authors were Boston Scientific representatives.
Boston Scientific funded this research.
The full study is available here.