Late balloon valvuloplasty safe and effective for patients with THV dysfunction
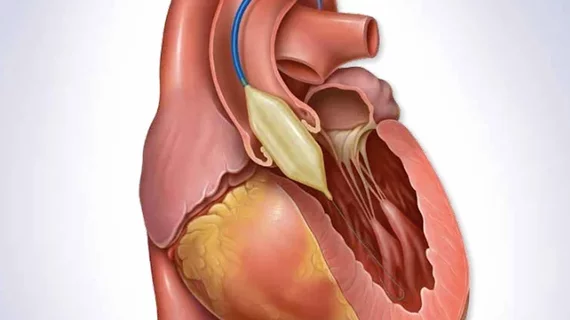
Balloon valvuloplasty months after implantation is a safe and effective treatment option for patients with transcatheter heart valve (THV) dysfunction, according to a new analysis published in the Journal of the American College of Cardiology.[1]
“Balloon valvuloplasty is a common component of THV procedures, performed immediately before, during, or immediately after THV implantation,” wrote lead author Mariama Akodad, MD, PhD, a cardiologist with the University of British Columbia and St. Paul’s Hospital, and colleagues. “In contrast, balloon dilatation late after THV implantation, as a staged procedure, has been described only rarely.”
The authors noted that the late balloon dilatation of THVs has been linked to numerous risks, including bioprosthetic leaflet injury, THV dislodgement, aortic root injury and stroke. However, they added, THVs are “frequently underexpanded” and “more aggressive dilatation may be required.” The group defined late balloon dilatation as “THV postdilatation performed as a staged standalone procedure or to facilitate the second THV implantation in underexpanded failed THV, as part of a redo TAVR procedure.”
Akodad et al. explored data from more than 1,000 patients who underwent a replacement of a native or bioprosthetic aortic, mitral, tricuspid or pulmonary THV at one of two facilities from 2016 to 2021. Out of that cohort, 30 patients underwent late balloon dilatation due to THV dysfunction; this included 22 aortic valves, two mitral valves, two tricuspid valves and one pulmonary valve. Dilatation occurred a median of 4.6 months after the initial THV implantation. For three patients, late balloon dilatation occurred before a planned redo TAVR procedure “to fully expand the underexpanded frame of the failed THV.”
Overall, the team found the mean transvalvular gradient decreased for all patients. Also, among all patients who presented with paravalvular leak (PVL) and were not scheduled to undergo redo TAVR, PVL was no longer detected following balloon dilatation.
“No patient had valve embolization, annulus rupture, coronary obstruction, or conversion to open heart surgery,” the authors added. “One patient had a major vascular complication when failure of percutaneous femoral hemostasis required surgical closure. Importantly, no patient had a leaflet tear or increase in valvular regurgitation following planned stand-alone balloon dilatation.”
The median follow-up period was 19.6 months, though two patients had died after one year. One of those patients died from cardiac arrest, and another died from cancer.
“Balloon postdilatation late after THV implantation may be a feasible and safe option in selected patients with THV underexpansion or undersizing to reduce transvalvular gradients, paravalvular leak, or facilitate redo THV procedures,” the authors concluded.
Related Structural Heart Disease Content:
Transcaval TAVR outperforms transaxillary TAVR when femoral access is not an option
4 promising heart failure therapies interventional cardiologists should keep an eye on
Reference: