AI predicts the likelihood of a common TAVR complication
Advanced artificial intelligence (AI) models can help cardiologists identify patients who may require a permanent pacemaker (PPM) after transcatheter aortic valve replacement (TAVR), according to new findings published in World Journal of Cardiology.[1]
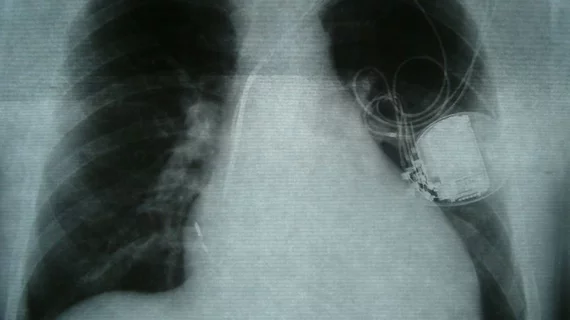
PPM implantation, the study’s authors explained, remains a relatively common complication after TAVR.
“PPM is associated with increased length of hospital stay and mortality,” wrote first author Pradyumna Agasthi, MD, a cardiologist at Mayo Clinic in Phoenix, and colleagues. “Additionally, advanced conduction defects requiring PPM implantation have been demonstrated to lead to worse functional capacity and clinical outcomes in patients with aortic stenosis (AS). The PPM requirement rate in TAVR is two to five-fold higher than in surgical aortic valve replacement.”
Agasthi et al. examined data from 1,200 patients who underwent TAVR due to severe symptomatic AS from 2012 to 2017. After excluding 236 patients who already had a pacemaker prior to undergoing TAVR, the group used supervised machine learning to run a PPM risk prediction analysis on the remaining 964 patients. The post-TAVR PPM rate among this cohort was 19.6% after 30 days and 26.7% after one year, numbers considered “similar to previous trials.”
The AI model used gradient boosting to focus on certain patient characteristics—including age and the presence of right bundle branch block, for example—associated with increased PPM rates.
Overall, the team’s AI model was found to be superior to an existing PPM risk score. The AI model’s area under the ROC curve (AUC) for predicting a patient’s 30-day and one-year risk of PPM were 0.66 and 0.72, respectively. The existing PPM risk score, meanwhile, had AUCs of 0.55 for 30-day risk and 0.56 for one-year risk.
Also, the team’s research found that “brachiocephalic to annulus distance-to-height ratio” was the single most significant predictor for post-TAVR PPM implantation, a finding that “has not previously been described in the literature.”
“This was primarily a feasibility study and is retrospective in nature, which restricts our ability for defining causal associations,” the authors added. “There is a need for prospective validation with an external cohort.”
Read the full analysis here.