Treating asymptomatic aortic stenosis with TAVR linked to significant benefits
Transcatheter aortic valve replacement (TAVR) is a safe, effective treatment strategy for asymptomatic, severe aortic stenosis (AS), according to late-breaking research presented Monday, Oct. 28, at TCT 2024 in Washington, D.C.
Lead investigator Philippe Généreux, MD, announced his team’s findings in front of a packed audience. Attendees cheered and roared with excitement as he revealed the study’s primary outcomes, an early sign that interventional cardiologists have been anticipating these results for quite some time.
Exploring the EARLY TAVR findings
EARLY TAVR included data from 901 patients 65 years old or older with asymptomatic, severe AS treated in the United States or Canada from March 2017 to December 2021. Patients were randomized to either undergo transfemoral TAVR with a balloon-expandable Edwards Lifesciences device or clinical surveillance.
The mean patient age was 75.8 years old, 69% were men and the mean Society of Thoracic Surgeons risk score was 1.8%. While a vast majority (83.6%) of patients faced a low surgical risk, the mean Kansas City Cardiomyopathy Questionnaire (KCCQ) score was 92.7, suggesting the cohort presented with a relatively healthy, symptom-free quality of life.
The study’s primary endpoint—a composite of all-cause mortality, stroke or unplanned cardiovascular hospitalizations—was seen in 26.8% of TAVR patients and 45.3% of clinical surveillance patients. This was primarily driven by a significant reduction in unplanned hospitalization—20.9% for TAVR, 41.7% for clinical surveillance—though early treatment was also associated with lower rates of all-cause mortality (8.4% vs. 9.2%) and stroke (4.2% vs. 6.7%).
To gain a better understanding of the benefits of early treatment, Généreux et al. also tracked KCCQ scores two years after randomization. A favorable health status—defined as being alive with a KCCQ score of at least 75 that had not decreased more than 10 points from baseline—was seen in 86.8% of TAVR patients and 68% of clinical surveillance patients.
Early treatment was also associated with improvements in left-ventricular and left-atrial health after two years. Meanwhile, changes in left ventricular ejection fraction as well as rates of new-onset atrial fibrillation and disabling stoke were comparable between the two treatment options.
After a median follow-up period of 3.8 years, 87% of patients in the clinical surveillance group had been chosen to undergo TAVR. Researchers noted that there were “no apparent differences in procedure-related adverse events” between patients who underwent early TAVR at the start of the trial and those who were moved over from clinical surveillance to TAVR during that follow-up period.
“Given the benefits observed and the lack of harm, early TAVR may be preferred to clinical surveillance in patients with asymptomatic severe AS, especially when combined with the challenges of timely symptom recognition and prompt treatment in real-world settings,” explained Généreux, director of the structural heart program at Morristown Medical Center’s Gagnon Cardiovascular Institute. “Not only is early intervention safe and effective, but it also prevents a decline in quality of life for those who later receive TAVR and could prevent the development of cardiac damage.”
These findings were simultaneously published in The New England Journal of Medicine.[1]
Additional insights from TCT
During a TCT press conference, Généreux emphasized that waiting for asymptomatic symptoms to become symptomatic before treatment may provide limited value. If you wait three to four years, he said, you create more opportunities for things such as cardiac damage or atrial fibrillation to occur.
“When you look at the pros and cons of waiting, there are not a lot of pros,” he said. “TAVR is so good, so seamless that even when you convert late, patients can still go home in the next day or two.”
One topic that came up during the press conference and then again after Généreux’s presentation was the comparable all-cause mortality rates between the TAVR and clinical surveillance groups. If early treatment is beneficial, one might wonder, shouldn’t the difference in mortality be more significant?
Généreux answered these questions by emphasizing that all EARLY TAVR participants were thoroughly followed and converted to TAVR within 30 days of the first signs of clinical symptoms. When clinicians are monitoring a patient with severe AS this closely, he explained, it is likely going to impact their odds of survival, regardless of the treatment strategy they were randomized to at the start of the study.
“We followed these patients,” he said. “We didn’t abandon them. Other trials … had crossover times of two years … this is where mortality occurs. With EARLY TAVR, we were really prompt.”
How might EARLY TAVR influence patient care going forward?
Professor Bernard Prendergast, chair of cardiology at Cleveland Clinic London and a consultant with St Thomas’ Hospital in Westminster, England, joined Généreux on the stage at TCT to explore the potential impact of these findings.
“The world has been waiting on the outcome of this trial,” he began, before reviewing some of the team’s key findings.
Prendergast went on to praise Généreux and the rest of the EARLY TAVR team for their efforts.
“This was an outstanding endeavor by the investigators,” he said. “The time from randomization to intervention was 14 days. The procedures were conducted with 0% cardiovascular mortality and low incidents of stroke, pacemaker, atrial fibrillation and major bleeding, the principle complications we all fear. Furthermore, the control group received outstanding clinical surveillance.”
Prendergast went on to summarize the long wait times patients encounter in much of the world. These are patients who can benefit from TAVR, he said, but they die on the waiting list instead of receiving the care they need. Prendergast sees the EARLY TAVR findings as a way forward.
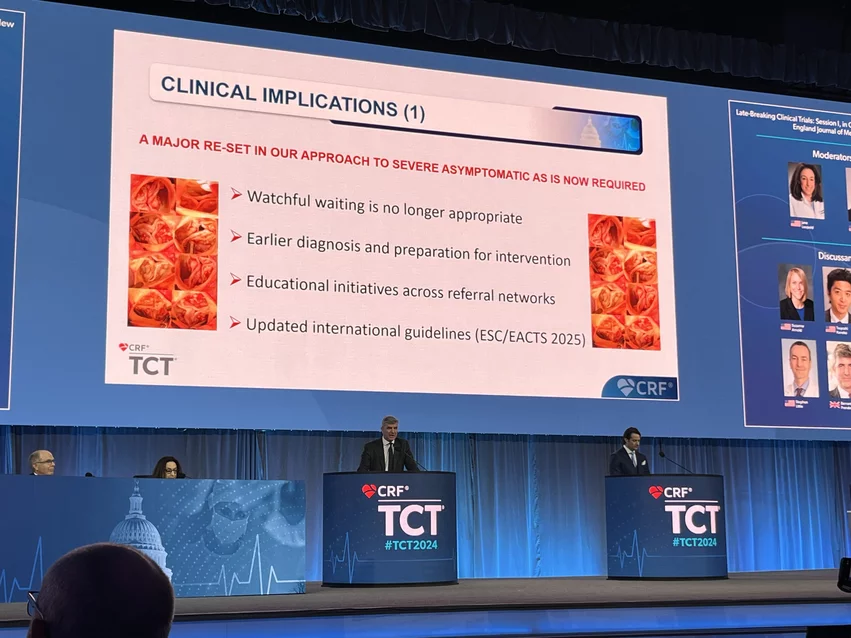
“A major reset in our approach to severe asymptomatic AS is now warranted,” he said. “The concept of watchful waiting is no longer appropriate and deserves reexamination. Patients require access to earlier diagnoses and they need to be prepared early for their interventional procedure.”
Edwards celebrates significance of EARLY TAVR
Edwards Lifesciences funded EARLY TAVR, and the company published a statement about the study’s “groundbreaking” findings.
“This is the first pivotal trial to generate evidence about the best strategy for disease management of severe aortic stenosis,” said Larry Wood, corporate vice president with Edwards Lifesciences and group president of TAVR and surgical structural heart. “EARLY TAVR challenges the current standard of care by definitively showing that patients who don’t have symptoms of severe aortic stenosis have a deadly disease that requires urgent treatment.”