Balloon-expandable valves deliver better short-term TAVR outcomes than self-expandable valves
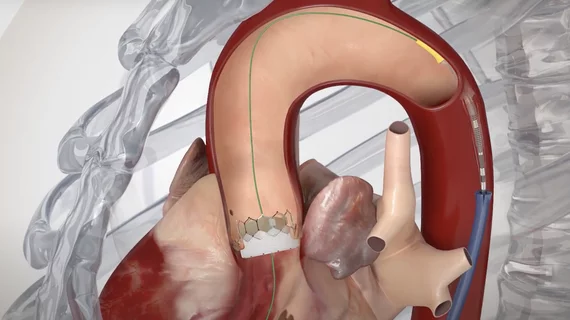
Transcatheter aortic valve replacement (TAVR) with a balloon-expandable valves (BEV) is associated with better 30-day survival rates than TAVR with a self-expandable valves (SEV), according to a new meta-analysis published in Frontiers in Cardiovascular Medicine.[1] The study included data from nearly 3,000 patients with severe symptomatic aortic stenosis.
“It is well-known that BEVs are associated with fewer pacemaker requirements than SEVs,” wrote first author Senguttuvan Nagendra Boopathy, MD, a cardiologist with the Sri Ramachandra Institute of Higher Education and Research in India, and colleagues. “But data regarding other hard-end points are scare.”
Boopathy et al. focused on data from six different studies. The cohort included 1,439 TAVR patients who received a BEV and another 1,496 TAVR patients who received an SEV. Transfemoral access was used for all TAVRs included in this analysis. A variety of different TAVR solutions were used, however, to help the study differentiate from studies that only focus on one vendor or directly compare one vendor with another.
The study’s primary outcome, all-cause mortality after 30 days, was seen in 2.2% of BEV patients and 4.5% of SEV patients. Cardiovascular mortality after 30 days, meanwhile, was seen in 2.5% of BEV patients and 4.2% of SEV patients. These statistics translated to a 51% relative risk reduction in all-cause mortality and a 42% relative risk reduction for cardiovascular mortality for TAVR with a BEV.
The 30-day rates of stroke, myocardial infarction, life-threatening bleeding events, major vascular complications, acute kidney injury and atrial fibrillation were all similar between the two groups. Device success was also similar between BEV and SEV patients.
The researchers did note that their work was linked to certain limitations. They performed a “study-level meta-analysis,” for example, and not a “patient-level meta-analysis.” Also, some of the studies included in their meta-analysis excluded patients with heavy calcification of the aortic annulus and left ventricular outflow tract, meanwhile, but other studies did not make those exclusions.
“Longer-term data are necessary to determine if the difference in outcomes persist and if the same effects are seen in lower risk patients,” the authors concluded.
Read the full meta-analysis here.