How CAD, PCI affect TAVR outcomes among men and women
Complex coronary artery disease (CAD) appears to be a have a more negative impact on transcatheter aortic valve replacement (TAVR) outcomes for woman than it does for men, according to new findings published in the American Journal of Cardiology.[1] As a result, women presenting with complex CAD may face a heightened risk of post-TAVR complications compared to men.
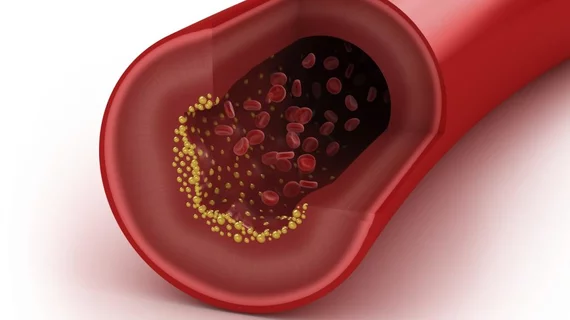
“It has been suggested that the complexity of CAD is a determinant of worse outcomes after TAVR,” wrote first author Lennert Minten, MD, of the department of cardiovascular sciences at Katholieke Universiteit Leuven in Belgium, and colleagues. “However, whether this applies equally to both genders is not known. Men are usually overrepresented in studies regarding CAD, and because there are inherent gender differences in the complex relationships between ischemia, angina and atherosclerosis, care should be taken when translating these results to the female population.”
Minten et al. examined data from more than 600 TAVR patients who were treated from 2008 to 2020. Fifty-three percent of those patients were men. All patients underwent CAD screening via coronary angiography prior to their TAVR procedure. They were evaluated using SYNTAX scores at that time, and those scores were used to identify patients with complex CAD.
Overall, after five years, survival was 62% among women and 59% among men. Cardiovascular mortality after five years, meanwhile, was 22% among women and 20% among men.
Women tended to be older at the time of their TAVR procedure and present with a higher left ventricular ejection fraction, higher aortic valve mean gradient and a lower aortic valve area. Angina rates were similar between the two groups, but women were less likely to present with obstructive CAD and less likely to have complex CAD.
“A possible explanation for the similar rates of angina despite less complex CAD in women might be a higher prevalence of underlying microvascular dysfunction, which is also known to be related to an increased rate of cardiovascular events,” the authors wrote. “Its prevalence needs to be studied further in the population with aortic stenosis (AS) together with the potential for coronary physiology to select lesions for revascularization.”
Percutaneous coronary intervention (PCI) and complete revascularization were both more common among women with CAD than among men with CAD. However, the team noted, mortality was still higher among women with complex CAD (40%) than it was among men with complex CAD (21%).
“In contrast to a generally accepted restrictive approach toward revascularization at the time of TAVR, women with AS who undergo TAVR might require enhanced attention concerning the treatment of CAD, primarily with optimization of medical treatment and potentially complemented with complete revascularization whenever feasible, particularly in complex CAD,” the authors concluded.
Bonus coverage: Click here to read about another TAVR-related study co-written by Minten.