New biomimetic TAVR valve, the first of its kind, linked to strong performance after 1 year
A new-look transcatheter aortic valve replacement (TAVR) device designed to mimic the patient’s native aortic valve is associated with strong safety outcomes and a “promising hemodynamic performance” after one year, according to new data published in EuroIntervention.[1]
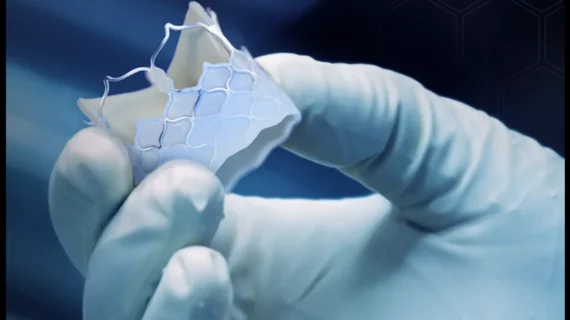
The DurAVR transcatheter heart valve (THV), developed by Minnesota-based Anteris Technologies, is a first-in-class device designed to move and perform like a healthy, pre-disease aortic valve.
“Traditional bioprosthetic aortic valves comprise of three separate pieces of flat tissue sutured together, which hinder complete valve opening and thus result in lower orifice areas and are potentially linked with abnormal flow patterns,” wrote first author Susheel Kodali, MD, an interventional cardiologist with Columbia University Irving Medical Center in New York City, and colleagues. “In contrast, the DurAVR THV is manufactured by molding a single-piece of tissue into the shape of a native aortic valve, facilitating a larger orifice area and near-normal flow patterns. This novel valve design, combined with the proprietary ADAPT tissue engineering anti-calcification process, is mounted on a short-frame, balloon-expandable platform with large open-cell geometry for coronary access.”
Kodali et al. examined data from the first 13 patients with severe, symptomatic aortic stenosis (AS) treated with the DurAVR THV. The mean age was 73.9 years old, and 10 patients were women. The cohort included “several challenging anatomies,” and the mean annulus size was 22.95 ±1.09 mm.
The TAVR procedure success rate was 100%, and there were no device-related complications. There was one access site complication—thrombosis of the external iliac artery and common femoral artery—and the issue was resolved the following day via surgery. In addition, one patient required a permanent pacemaker six days following treatment. Other than those incidents, however, the valve was associated with a strong safety profile. There were no deaths, myocardial infarctions, strokes or bleeding events after 30 days, six months or one full year.
“There were no device-related complications, reoperation or reinterventions reported or changes in QRS and PR intervals observed throughout follow-up beyond the patient who was implanted with the permanent pacemaker,” the authors added. “Additionally, no neurological dysfunction or acute kidney injury were recorded.”
According to transthoracic echocardiography (TTE) results, there was mean effective orifice area of 2.0±0.17 cm2, mean indexed effective orifice area of 1.14±0.15 cm2/m2, mean pressure gradient of 9.02±2.68 mmHg, and mean Doppler velocity index of 0.53±0.1. Additional TTE assessments confirmed that the device’s encouraging hemodynamic performance was sustained after six months and one year. Researchers also examined post-operative CT results, noting that there were no calcifications after 30 days and leaflet mobility was normal. Hypo-attenuated leaflet thickening (HALT) limited to the base was seen in one patient, and 50-75% HALT was seen in another patient. Oral anticoagulation therapy was prescribed, resolving the issue for the patient with 50-75% HALT.
Overall, the research team concluded, these one-year results offered plenty of reasons to be encouraged about the THV’s performance.
“The preliminary observations provided here will serve as a basis for future powered clinical trials to gain a better understanding of how the acute benefits of a biomimetic design (hemodynamics and normalized flow) impacts on quality of life, durability, myocardial recovery, myocardial remodeling and aortopathies in the long-term treatment of AS,” the authors wrote.
Read the full analysis here. These findings were also presented as part of EuroPCR 2023, the annual meeting of the European Association of Percutaneous Cardiovascular Interventions.