Permanent pacemaker implantation after TAVR increases healthcare costs by $24,000 per patient
Implanting a permanent pacemaker (PPM) after transcatheter aortic valve replacement (TAVR) is costing health systems an average of more than $23,000 per patient, according to new findings published in Cardiovascular Revascularization Medicine.[1] This includes the price of the device, the implant procedure and other costs not directly related to patient care.
“There is a lack of contemporary and multicenter evidence on the direct and indirect costs associated with PPM implantation post-TAVR, which has meaningful implications for the economics of TAVR procedures,” wrote first author Christopher L. Brown, MD, an interventional cardiologist with the Swedish Heart and Vascular Institute in Seattle, and colleagues. “Hospital accounting practices of direct and indirect costs measure per-case profitability, which informs decision-making for hospital investment in new or expanded TAVR programs.”
Brown et al. explored data from more than 7,800 patients who underwent TAVR from 2016 to 2020 at one of 16 U.S. hospitals. Patients with a pacemaker at baseline were excluded. Overall, 8.5% of patients required a PPM after TAVR.
Nearly half (49.9%) of the patients who required a PPM after TAVR presented at a low surgical risk. Meanwhile, 32.9% of patients presented at an intermediate risk, 13.1% presented at a high surgical risk and 4.1% presented at a prohibitive surgical risk. PPM patients were more likely to be white and male, and the average age was 81.7 years old.
On the financial side of things, even after adjusting for patient and hospital characteristics, requiring a PPM implantation after TAVR was associated with an average of $23,588 per patient. This includes $14,466 in direct costs—the price of the device, the physicians and so on—and another $9,157 in indirect costs such as IT services and capital expenses.
As one might expect, patients who required a PPM were also associated with longer lengths of stay and additional time spent in the intensive care unit. Brown and colleagues also noted that these patients were not associated with a higher risk of 30-day readmission.
“Because of the overall clinical and cost burden of PPM implantation post-TAVR, we believe that a focus on reduction of PPM implantation post-TAVR is of vital importance to the financial solvency of hospital cardiovascular programs nationally,” the authors wrote. “We believe that attention to modifiable ways to reduce PPMI rates is critical, and continued research efforts are important to help clarify best practices to achieve the lowest PPMI possible.”
Edwards, which has its own line of TAVR and structural heart disease devices, did fund this analysis, and multiple Edwards representatives were listed as study co-authors. However, Brown reported no financial or consulting relationship of any kind with the large healthcare technology vendor.
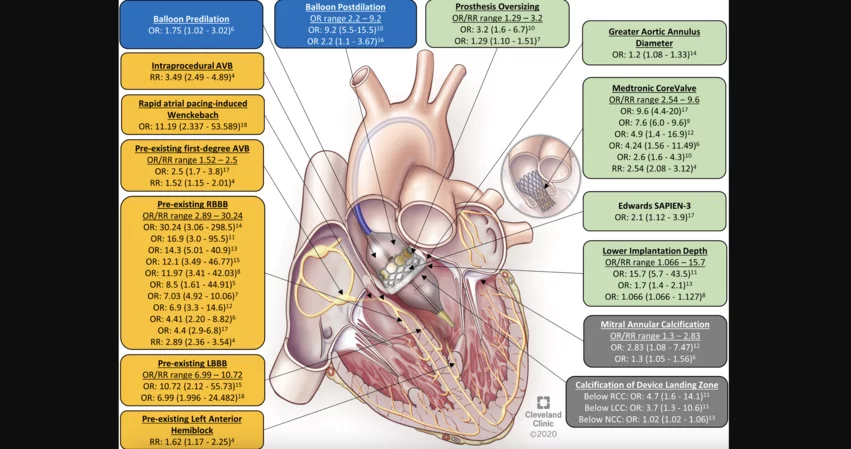
Click here for a 2021 state-of-the-art review from the American College of Cardiology focused on PPM implantation after TAVR.