Transcaval TAVR a safe, effective alternative for patients with severe AS
Transcaval transcatheter aortic valve replacement (TAVR) appears to be a safe, effective alternative for patients with severe aortic stenosis (AS) when a transfemoral approach is not recommended, according to a new meta-analysis published in The Canadian Journal of Cardiology.[1]
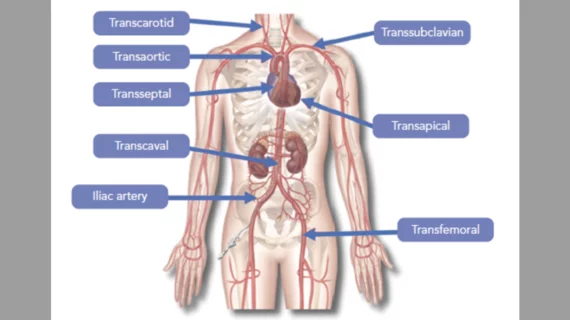
“While the transfemoral approach is the preferred vascular access for TAVR, it may be unfeasible in approximately 5-10% of patients due to anatomical challenges such as small vessel size, marked vessel tortuosity or extensive calcification of the iliofemoral vasculature,” wrote first author Adil Salihu, MD, a cardiology resident with Lausanne University Hospital in Switzerland, and colleagues. “To address these challenges, various alternative vascular access routes have been developed, with the transcaval access being the latest advancement. Setting itself apart from previous alternative accesses, such as the transapical approach that necessitates a direct access to the left ventricular apex, or methods involving percutaneous or surgical puncture and access of the arterial vascular system, the transcaval approach involves accessing the abdominal aorta through the adjacent inferior vena cava.”
Salihu et al. tracked data from a more than 400 patients who underwent transcaval TAVR for severe AS. The mean patient age was 76.8 years old, and a majority (57%) of patients were women. While 92% of patients presented with hypertension, ischemic heart disease was seen in 83% of patients and artery disease in the lower extremities was seen in 69%. The mean left ventricular ejection fraction was 51%, mean aortic valve gradient was 40 mmHg and mean aortic valve area was 0.7 cm2. All patients were participants in one of eight studies included in the team’s meta-analysis.
Transcaval TAVR was associated with a success rate of 98.5%. All-cause mortality was 6.4% after 30 days and 14.4% after one year. While the 30-day rehospitalization rate was 4.4%, post-TAVR rates of stroke, transient ischemic attack and major vascular complications were 3.9%, 8.5% and 10.1%, respectively. In addition, vascular complications appeared to grow less and less common as transcaval TAVR became more common and the technology evolved.
The authors did note that transcaval TAVR appears to be associated with a higher mortality rate than transfemoral TAVR, “likely related to variations in population characteristics such as comorbidity burden and a high surgical risk profile.” In addition, transcaval TAVR was linked to a “relatively high” permanent pacemaker rate (15.3%), which “might be attributable to the high-risk nature of the studied population, many of whom possibly had preoperative conduction disease.”
Overall, however, the team concluded that transcaval TAVR shows potential to be a “viable alternative” for patients who are not a good fit for transfemoral access.
“The decision to perform transcaval TAVR should be guided by considerations such as patients' vascular anatomy, comorbidities, and the expertise of the operator,” the authors wrote. “This decision-making process should be individualized, highlighting the importance of operator proficiency, particularly given the relatively recent emergence of transcaval TAVR as a procedure, primarily performed in high-volume and experienced centers.”
Click here to read the full meta-analysis in The Canadian Journal of Cardiology, an official publication from the Canadian Cardiovascular Society.