Clot flow, location predict effectiveness of alteplase for stroke care
Certain characteristics predict how responsive a blood clot will be to intravenous alteplase, according to research published Sept. 11 in JAMA—knowledge that may help clinicians more efficiently triage patients with acute ischemic stroke.
Lead author Bijoy K. Menon, MD, MSc, with the University of Calgary in Canada, and colleagues conducted a prospective study of 575 patients from 12 centers spanning three continents. All patients underwent head and neck CT angiography (CTA) at baseline and had a visible intracranial thrombus.
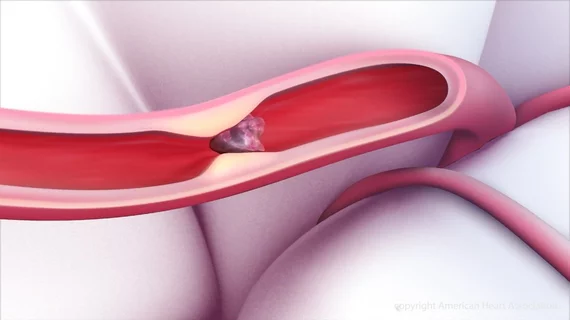
Overall, 27.3 percent achieved successful recanalization upon follow-up imaging within six hours, including 30.4 percent who received IV alteplase and 13.3 percent who did not. Among the patients who received the thrombolytic drug, the following factors were associated with increased odds of recanalization, or a reopening of the occluded vessel:
- Time from treatment to recanalization assessment: 28 percent increased odds of recanalization for every 30 minutes.
- More distal thrombus location: 5.61-fold increased odds of recanalization.
- Higher residual flow, or thrombus permeability: 7.03-fold increased odds of recanalization.
On the other hand, male sex was the only factor associated with increased odds of recanalization among patients who didn’t receive alteplase.
“There is … a clear need to predict with clinical and imaging criteria which patients are most suitable for transfer to a comprehensive stroke center for endovascular therapy (versus) who can remain at the primary stroke center,” Menon et al. wrote. “Patients with factors associated with thrombus responsiveness to alteplase (e.g., thrombus permeability) may not require transfer because they will recanalize with intravenous alteplase.”
Early recanalization with either endovascular therapy or alteplase is associated with improved outcomes for stroke patients. Because a transfer to a thrombectomy-capable stroke center may take significantly longer than treatment at the primary center, the authors said it is important to have reliable methods to determine when such a transfer is unnecessary.
Among other limitations, Menon and colleagues noted they didn’t have data on clinical outcomes related to thrombus recanalization.