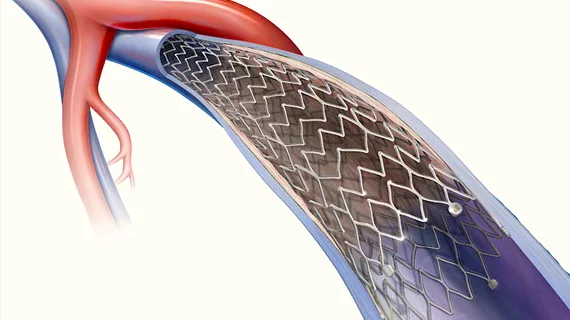
Office-based cath lab setting proves safe for iliac vein stenting
In recent years, more and more interventional procedures have been moved from conventional hospital-based cath labs to outpatient office-based labs (OBLs). The advantage of these labs is they can streamline operations and reduce costs, especially for less complex interventions in both veins and arteries. OBLs pose both a business opportunity and threat to procedure volumes in some healthcare systems. However, studies need to show that procedures performed in these labs can be done safely and without the need for hospital-based surgical backup.
A new study January 2022 issue of the Journal of Vascular Surgery: Venous and Lymphatic Disorders, for example, shows evidence that iliac vein procedures can be performed in OBLs with an extremely low rate of complications.[1] The journal is a publication of the Society of Vascular Surgery (SVS).
The retrospective study of 1,223 iliac vein cases performed in three office-based laboratories showed a major complication rate of 0.41%, suggesting these procedures are safe and well-tolerated in this setting.
“Because OBLs are not regulated to the same degree as in-patient facilities or ambulatory centers, questions have been raised regarding patient safety and outcomes in this environment," explained corresponding author Levan Sulakvelidze, BS, from the Center for Vascular Medicine in Greenbelt, Maryland. “The safety profile of iliac vein stenting in the OBL setting has not been thoroughly evaluated. The purpose of the present study was to evaluate the complication rate and safety profile of this procedure when performed in an OBL.”
Sulakvelidze and colleagues reviewed prospectively collected data from 1,104 patients who underwent a total of 1,223 iliac vein stents in OBL centers.
Three patient groups were studied based on presentation:
• Lower extremity symptoms alone: 305
• Pelvic symptoms alone: 91
• Combination of the two: 827
Trained nursing personnel, under the supervision of the attending interventionalist, administered conscious sedation to all patients. Typical dosing involved 1 mg of midazolam and 50µg of fentanyl. Excluded from this setting were patients with a significant cardiac or pulmonary risk, a history of severe airway issues, morbid obesity or complex venous lesions.
There were no deaths and no complications related to the sedation rendered.
The total complication rate was 7.8%. This included five major complications (0.4%), defined as complications that required hospitalization for allergic reaction, arrhythmia, chest pain or stent occlusion. There were 90 minor complications, mainly involving minor access bleeding (39) and hematoma (31).
“In the study, because most of the complications were considered minor, including suspected over-reported hematomas, we have presented strong evidence that demonstrates iliac stenting performed in the OBL setting is safe," Sulakvelidze said. “Given these promising results, we recommend all OBLs become Joint Commission (JCAHO)-certified and include quality assurance efforts to maximize patient safety.”
Patient safety and quality care remain the most important goals of any procedure rendered by a vascular interventionalist, said JVS editors. “This important study confirms that both can be achieved in the OBL setting for patients who require iliac vein stenting.”
Related OBL Content:
Championing Alternative PAD Access in the Office-based Lab
SCAI unveils new cath lab guidelines at annual meeting
Reference: