T-cells in arterial plaque could signal stroke risk
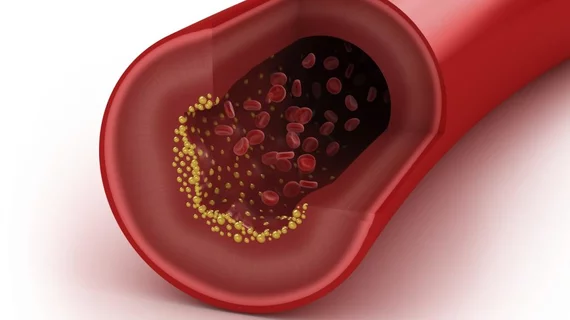
Researchers have linked a specific type of immune cell found in arterial plaque to increased probability of a stroke or mini-stroke.
Chiara Giannarelli, MD, PhD, and colleagues’ study dissected and scrutinized human plaque in an effort to identify markers that might flag a patient as high-risk for vascular dysfunction, according to a release. The researchers presented their findings at the American Heart Association’s Vascular Discovery Scientific Sessions in Boston on May 14.
“Despite decades of research, we don’t know how to predict and prevent plaque from rupturing in the arteries,” Giannarelli, an assistant professor at the Icahn School of Medicine at Mt. Sinai Medical Center in New York, said in a release. “Most of the research has involved looking at human tissue under the microscope. This has helped us better understand many features of ruptured plaque, but little is known about how and which individual cell type contribute the most to ruptures causing stroke or heart attack.”
Giannarelli’s team recruited 38 patients, on average 72 years old, who they studied in two separate groups. All patients underwent a procedure to correct carotid artery stenosis, and some had experienced a recent stroke or mini-stroke while others presented with no symptoms.
The researchers first looked at a subset of 15 patients, using mass-cytometry to break down the basic cellular makeup of their plaque tissue. They found T-cells—lymphocytes that play a central role in immune response—dominated the plaque.
Giannarelli et al. then conducted a second mass-cytometry analysis and evaluated gene expression in the remaining 23 patients, finding similar results. T-cells continued to dominate advanced plaques, and the team said CD4-positive effector memory cells, a subtype of T-cells, were more common in patients who’d had a previous stroke or mini-stroke.
Giannarelli said that though her team’s study is limited in its small sample size, it does highlight the fact that there’s localized inflammation driven by T-cells in atherosclerotic plaque that isn’t related to any systemic immune response. T-cells found in plaque were unconnected to those found in patients’ blood samples.
“Our study found that plaque from stroke patients is full of T-cells that are part of the adaptive immune system, a specialized second-line of defense in the body,” Giannarelli said. “This may help us eventually identify targets for new immune therapies for the late stages of atherosclerosis.”