Thrombolysis vs. surgery for prosthetic valve thrombosis
Thrombolysis is an effective alternative to surgery for patients with prosthetic valve thrombosis (PVT), according to new findings published in the Journal of the American College of Cardiology.[1]
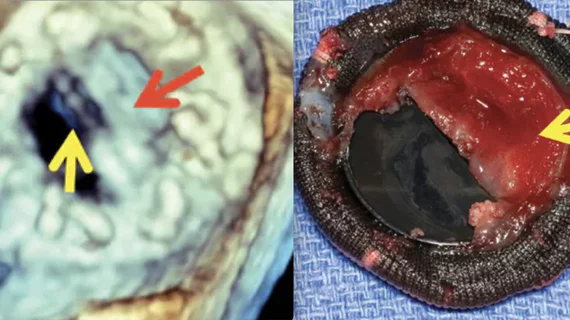
Surgery is often recommended for the management of PVT patients, but mortality rates can be as high as 18%. Meanwhile, multiple research teams have found that thrombolysis involving the slow (6 hours) or ultraslow (25 hours) infusion of a low-dose tissue plasminogen activator (t-PA) can help some patients avoid surgery altogether.
To learn more about the short-term safety and effectiveness of thrombolysis, a team of researchers focused on data from 158 patients newly diagnosed with obstructive PVT from December 2013 to December 2020. The median patient age was 49 years old, and 65.2% were women.
While 83 patients underwent thrombolysis for their obstructive PVT, 75 patients were treated with surgery. Only patients who met the criteria for both treatment options were included in this analysis. The choice between thrombolysis or surgery was made by a heart team that featured a cardiologist, a cardiovascular surgeon and an anesthesiologist. The patient was also involved in making the final decision.
Thrombolysis patients either underwent six-hour infusions of t-PA, repeated up to six times in total, or a 25-hour infusion of t-Pa, repeated up to eight times in total.
“For patients developing headache, suspicious symptoms of bleeding, or embolism during t-PA infusion, the treatment was interrupted until the patient was comprehensively evaluated with relevant consultations and imaging tools,” wrote first author Mehmet Özkan, MD, a cardiologist at Ardahan University in Turkey, and colleagues. “If a major complication was confirmed, subsequent management was individualized considering both the severity of the complication and the residual valvular obstruction.”
Overall, the team found, thrombolysis had a success rate of 90.4%. The treatment was viewed as a success when clinicians saw complete improvements in valve hemodynamics, a reduction in the major diameter and/or area of the thrombus by at least 75% and symptomatic improvements.
The three-month mortality rate was 2.4% after thrombolysis and 18.7% after surgery.
Major complications, meanwhile, were seen in 6% of patients after thrombolysis and 41.3% of patients after surgery. Minor complications were seen in 8.4% of patients after thrombolysis and 38.7% of patients after surgery.
“Slowly administered infusions of t-PA are a safe and effective alternative to surgical therapy in selected patients with obstructive mechanical heart valve prostheses,” the authors wrote.
The team, however, did call for larger randomized trials to help guide the treatment of PVT patients moving forward.
Related Vascular and Endovascular Content:
DOACs may reduce the risk of dementia among AFib patients by 50%
PCI boosts survival for ischemic HF patients with moderate-to-severe mitral regurgitation
Evolocumab limits adverse cardiovascular outcomes among PCI patients
Distal radial access consistently lowers risk of artery occlusion during PCI
FDA Roundup: AAA EVAR recommendations, key approvals in stroke care and interventional cardiology
Reference: