Watchman thrombi occur in 3.7% of implants, heighten stroke risk
Watchman-related thrombi developed in 3.7 percent of patients who were implanted with the device, resulting in a threefold risk of stroke or systemic embolism, according to a meta-analysis of clinical trials and registries published online May 11 in Circulation.
What’s more, researchers found 47 percent of the embolic events occurred within one month of the device-related thrombus (DRT) being detected, suggesting a temporal relationship between DRT and stroke. About two-thirds of the embolisms occurred within six months of DRT being detected.
“Given the ramifications of DRT, a judicious surveillance strategy using periodic transesophageal echocardiography should be considered, particularly when risk factors for DRT are present,” wrote senior author Vivek Y. Reddy, MD, with the Icahn School of Medicine at Mount Sinai, and colleagues. “Anticoagulation should promptly be resumed when DRT is detected to potentially decrease the risk of subsequent ischemic stroke.”
Individuals with previous strokes or transient ischemic attacks, permanent atrial fibrillation (AFib) and vascular disease all showed more than double the risk of developing DRT. Other independent predictors were a larger left atrial appendage (LAA) diameter and a lower left ventricular ejection fraction.
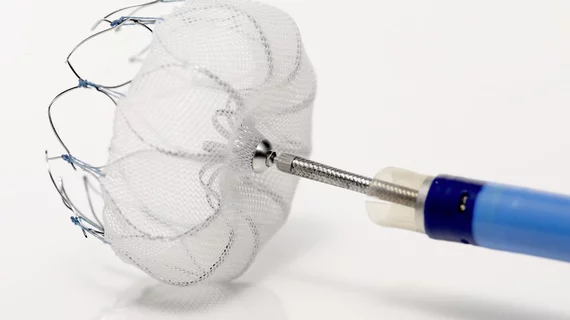
Reddy and coauthors pooled patients from two prospective studies and two registries who had Boston Scientific’s Watchman device implanted. The device occludes the LAA and is indicated as an alternative to warfarin for patients with AFib and a moderate to high stroke risk who may not tolerate long-term anticoagulation.
Although the device has been linked to reduced stroke risk, DRT has been reported and was found in this analysis to triple the risk of stroke or systemic embolism when compared to patients who didn’t develop DRT. In all, the meta-analysis included 1,739 patients, 65 of whom developed stroke.
Despite DRT carrying a higher stroke risk, there was no significant association with all-cause mortality. Also, the absolute number of strokes linked to DRT remained relatively low, the authors pointed out.
“The temporal relationship between DRT detection and the occurrence of stroke is suggestive of a causative relationship; however, it is important to note that the majority of patients with DRT (73.8%) did not experience a stroke/systemic embolism and the majority of strokes/systemic embolisms (86.6%) occurred in patients who never manifested a DRT,” Reddy et al. wrote.
The authors also noted that the overall stroke rate in their study group was similar to what would be expected of a cohort with the same CHA2DS2-VASC risk score (4.0) treated with anticoagulants.
Still, they said additional echocardiograms could be considered in patients with the aforementioned risk factors for DRT, and added the initial echo could be pushed back from six weeks to four months considering DRT is most likely to occur after post-procedural anticoagulation therapy has stopped.
The researchers called for future studies to evaluate different oral anticoagulants for their potential to resolve DRT.
Reddy reported receiving research grant support and consultant fees from Boston Scientific, which funded all the trials and registries included in the meta-analysis.