Physician review boosts accuracy of smartwatch AF detection algorithm
A smartwatch algorithm reliably differentiated atrial fibrillation (AF) from sinus rhythm among patients scheduled for elective cardioversion, showing the technology’s potential to prevent unnecessary procedures.
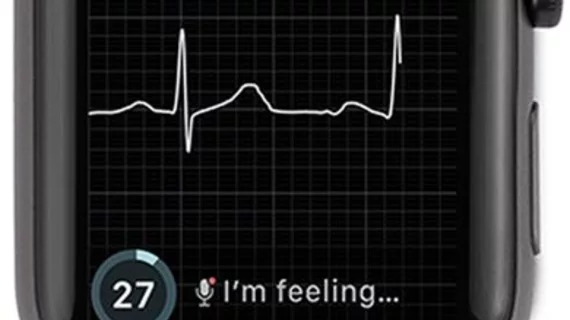
Researchers at the Cleveland Clinic studied the algorithm among 100 patients with known AF. Before cardioversion, each patient had simultaneous electrocardiograms (ECG) and Kardia Band (KB) recordings measured. The KB, developed by AliveCor, allows patients to take a rhythm strip using an Apple Watch application and is paired via Bluetooth with a smartphone.
Based on the results of the recording, a user may be alerted to the presence of AF, and readings are sent directly to a physician.
Compared with physician-interpreted ECGs, the KB algorithm identified AF with 93 percent sensitivity and 84 percent specificity. When electrophysiologists reviewed the KB readings, AF detection improved to 99 percent sensitivity and 83 percent specificity.
A total of 169 simultaneous ECG and KB recordings were studied, with 57 of them being noninterpretable by the KB due to the recordings being too short, too noisy or the heart rate too fast or too slow. But even for these unclassified measurements, physicians achieved a specificity of 100 percent and a sensitivity of 80 percent.
Lead author Joseph M. Bumgarner, MD, and colleagues noted the accuracy of the KB was similar to that of previously studied implantable loop recorders.
“AF is a good example of a relapsing condition that requires frequent monitoring of clinical endpoints to assess the efficacy of treatment choices and plan future interventions,” they wrote in the Journal of the American College of Cardiology. “The KB is the first smartwatch accessory cleared by the FDA and available to the general public without a prescription that claims to instantaneously detect AF and transmit this information to a patient’s treating physician.”
Notably, 8 percent of patients who presented for cardioversion in the study were already in sinus rhythm—a finding identified by the KB and confirmed upon physician review. These patients didn’t undergo cardioversion.
“Although this study was not powered to assess the financial consequences of cancelled CVs, it is reasonable to conclude that a measurable number of resources were forfeited by both the patient and the health care system in anticipation of a procedure that was ultimately deemed unnecessary once (sinus rhythm) was confirmed,” the authors wrote. “As data from the KB can be reviewed remotely, the resources used in preparation of these patients’ cancelled CVs could have been saved. … Our study suggests the potential use of these products to provide more effective health care delivery.”
Limitations of the study include its single-center design, small sample size, heavily male (83 percent) population and that all patients were using the KB for the first time but were instructed how to use it immediately beforehand. The accuracy and quality of the recordings may be worse in a non-guided, ambulatory setting but possibly better with patients who are more familiar with the device, Bumgarner and colleagues pointed out.
Although the researchers concluded unnecessary cardioversion visits could be avoided with the KB, Theofanie Mela, MD, said in an accompanying editorial the more important question is how clinicians can use information from wearable devices to prevent arrhythmic episodes and strokes.
“Numerous studies have involved ambulatory monitoring … and they confirmed that the more we look for AF the more we find it,” wrote Mela, an electrophysiologist with Massachusetts General Hospital and Harvard Medical School. “It seems that technology has clearly progressed faster than the medical world’s ability to address the challenging management questions.”
Randomized trials are underway evaluating anticoagulation strategies for their abilities to prevent stroke in the AFib population, she noted, but the results likely won’t be published for several years.
“During that time, we will certainly have the benefit of utilizing these novel algorithms and devices to diagnose unrecognized or recurrent AF and apply the existing evidence and our best judgment to manage our patients,” Mela wrote.