Medicare will now cover weight loss drug semaglutide if taken for heart benefits
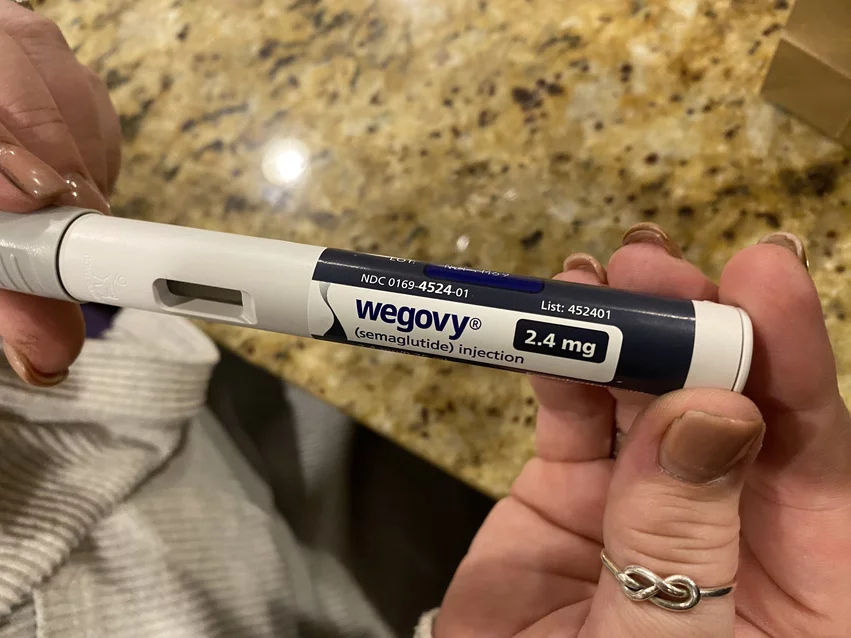
The U.S. Centers for Medicare and Medicaid Services (CMS) has announced that semaglutide, Novo Nordisk’s obesity drug sold under the brand name Wegovy, will be covered by Medicare if prescribed for its heart health benefits. The news represents a meaningful policy shift for CMS—up to this point, Medicare prescription drug plans have not covered medications designed to help patients lose weight.
The announcement from CMS comes just weeks after the U.S. Food and Drug Administration (FDA) approved 2.4-mg doses of semaglutide as a way reduce the risk of major adverse cardiovascular events in patients who are overweight or obese and present with cardiovascular disease (CVD). This was the first time the FDA had approved an obesity drug for its heart benefits, and the agency even issued a statement highlighting the moment’s historical significance.
CMS has now responded to that historic approval by updated its policy on covering weight loss drugs for Medicare patients. An agency representative explained the new stance in a statement sent to Cardiovascular Business.
Semaglutide (Wegovy) is a GLP-1 receptor originally developed to treat diabetes and now approved to help adults lose weight and reduce their risk of adverse cardiovascular events. Medicare said it is now willing to pay for the drug to help reduce cardiovascular risks, and is the first weight loss drug to receive coverage from CMS.
“CMS has issued guidance to Medicare Part D plans stating that anti-obesity medications that receive FDA approval for an additional medically accepted indication can be considered a Part D drug for that specific use,” the spokesperson explained, adding that Medicare coverage “is still not available” to patients only taking the drug to lose weight.
Medicare Part D plans are able to make these moves at any point in the year as needed. Separate CMS approval is not needed if coverage parameters are being updated to stay in step with this policy.
“Part D plans may consider using prior authorization for these products to ensure they are being used for a medically accepted indication,” the CMS spokesperson added.