Why the business side of cardiology was a key focus at ACC.24
At ACC.24, the annual conference of the American College of Cardiology (ACC), the spotlight was not solely on medical breakthroughs and treatment modalities, but also on finances, cardiologist reimbursements, staffing and more. ACC doubled the number of business-related sessions at this year's meeting, and economics and business finance literacy are more important than ever as reimbursements continue to decline.
Cardiovascular Business spoke with Alison Bailey, MD, chief of cardiology at Centennial Heart at Parkridge Medical Center, and a physician director of cardiovascular disease for HCA Healthcare. She co-chaired the series of sessions addressing the business aspects of cardiology.
"We think it's really important. We did four sessions over the course of two days really talking about the basics of cardiovascular business. And so our goal was really to get all of our members to understand the basics of how funds flow, how we're reimbursed and how healthcare works in the United States so that we can build sustainable systems not only for our patients, but also for our care teams," Bailey said.
Bailey emphasized the critical need for cardiologists to understand the financial dynamics of their profession, noting that while they excel in medical interventions, financial literacy often takes a back seat in their training. With the healthcare landscape constantly evolving, she stressed the importance of advocacy and active engagement in shaping policies that affect reimbursement and practice sustainability. Despite being very intelligent overall and highly trained, she said cardiologists generally have a very low understanding of how hospitals and physicians are actually reimbursed and the factors involved.
"I think most of us have some baseline understanding ... a patient comes to the hospital, we do something to a patient, whether that's an imaging study or an office visit, and we get reimbursed. But I don't think most people have a good grasp," Bailey said.
Session attendees gained insights into value-based care models, the impact of quality metrics on patient outcomes, and the future of medicine amidst emerging trends like private equity involvement and the rapid change in how most cardiologists are employed.
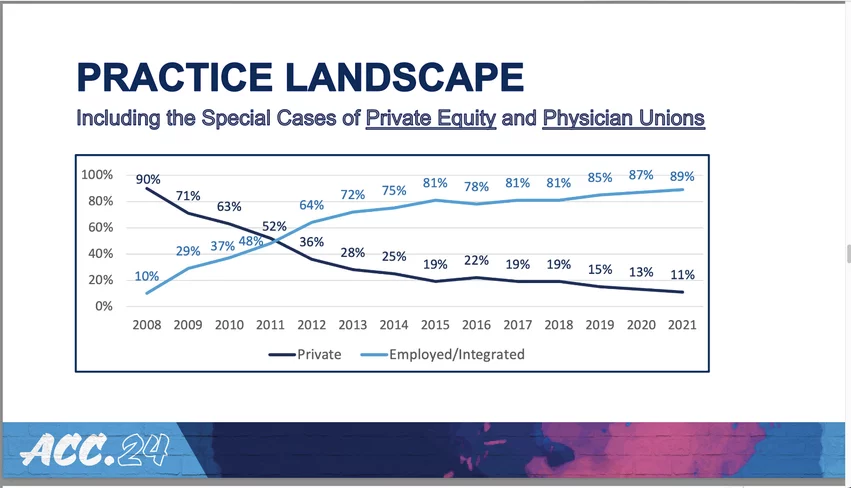
In the past decade, there has been a major shift in how cardiologists are employed. It changed from 90% in private practice in 2008 to rapidly being flipped completely opposite due to changing government policies and the economics involved in reimbursement. This was a key slide in the business of cardiology keynote by MedAxiom CEO Jerry Blackwell.
The changing cardiology employment and ownership models
One of the key concerns addressed in the sessions was the shifting employment landscape for cardiologists. Over the past decade, there has been a significant transition from private practice to hospital employment. In 2008, Bailey said 90% of cardiologists were in private practice, but due to changing reimbursement policies making payments lower for doctors and increasing for hospitals, in 2021 that number dropped to just 11%. 89% of cardiologists are now employed by hospitals or integrated care networks.
"That has consequences that go with it," Bailey said.
She highlighted the implications of this shift, including the importance of understanding the financial dynamics and the challenges it poses to cardiologists who often lose their autonomy. This can contribute to physician burnout and adds to the ongoing healthcare workforce shortages.
"We're also seeing huge challenges in nursing. In the recent survey, only one in 10 of nursing school students see doing bedside nursing in their future. So the way that we deliver healthcare in this country is not appealing to the younger generations and people aren't wanting to do it forever. So we need to figure out how we change that and how we make it more palatable. We want to be pushing people out of cardiology at the end of their career, not having them stop work at 55," Bailey explained.
Need for more cardiologists to get involved in advocacy efforts
One of the biggest factors impacting reimbursements and the hoops cardiologists must jump through to get paid boils down to government policies. For this reason, Bailey said advocacy is extremely important and urged more cardiologists to get involved. Politics and healthcare economics have emerged as intertwined factors driving the future of cardiology practice. Bailey emphasized the need for physicians to engage in advocacy efforts to influence healthcare policy positively.
"I don't think people understand that if we're getting cut by Medicare, it translates into loss of innovation, translates into loss of new procedures for our patients, and buying new tools to improve healthcare outcomes. And then we get bogged down in the everyday business of what we do with electronic medical record systems that really don't improve our lives and don't improve our patient lives, but increase the administrative burden. We have prior authorizations and all these other things that we have to deal with, and I already don't have enough hours in the day to take care of my patients," Bailey said.
ACC's advocacy arm, the HeartPAC, was highlighted in sessions as a crucial platform for cardiologists to voice their concerns and advocate for policies that promote innovation and improve patient care. In addition to ACC, most other cardiology societies also have advocacy groups where cardiologist can make their voices be heard in Washington and in state legislatures.