FDA Commissioner Robert Califf calls on cardiology to address health inequities and combat misinformation
U.S. Food and Drug Administration (FDA) Commissioner Robert Califf, MD, who is a cardiologist, spoke at the opening session of the American Heart Association (AHA) 2022 Scientific Sessions about the need for doctors and health systems to step up to address two major problems. He said public misinformation about healthcare has become a major issue and clinicians need to push back to prevent hospital over crowding and further COVID deaths. Califf also stressed the need to address health disparities, as U.S. healthcare costs continue to rise, while the average life expectancy continues too drop compared to other developed nations.
"We all sort of know what to do, but we are not doing it," Califf said.
Innovation is needed to address severe health disparities
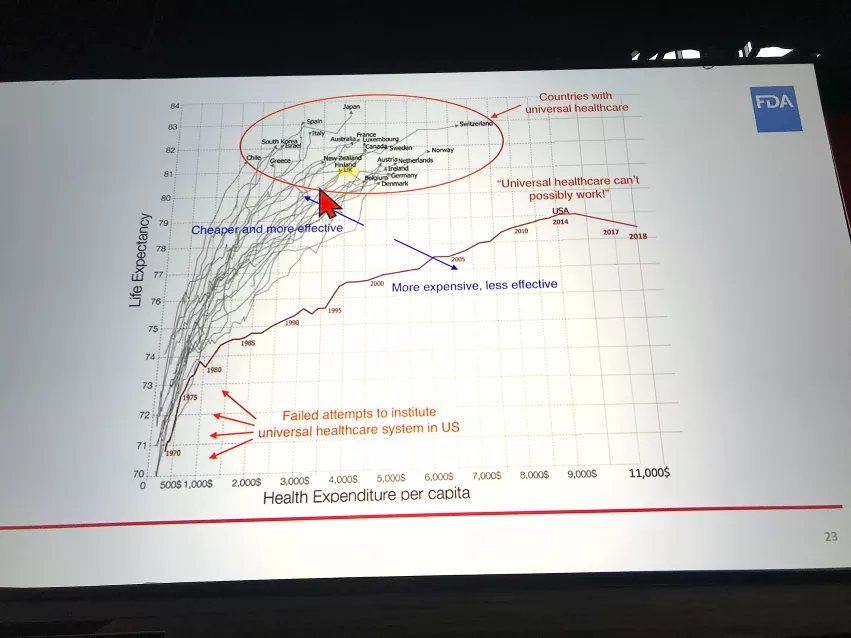
"Innovation is an area where we are not getting the job done," he said. While the U.S. has a large amount of new technology and is the source of many healthcare innovations, this has not impacted U.S. healthcare statistics. And the U.S. is falling behind other nations that spend less and have better health outcomes and life expectancy than Americans.
He showed a graphic measuring 23 developed countries with universal healthcare compared to the U.S. in terms of life expectancy and health expenditure per capita. It showed all of those countries out-perform the U.S. while spending less on healthcare. All of the foreign countries had average life expectancies above age 80 and a per-capita health expenditure of about $4,500. Califf pointed out the U.S. has an average life expectancy age of about 78.4 today and is spending about $11,000 per capita on healthcare. And, the life expectancy actually dropped between 2014 and 2018, the last years of the graphic.
"China passed us this year in life expectancy," Califf pointed out.
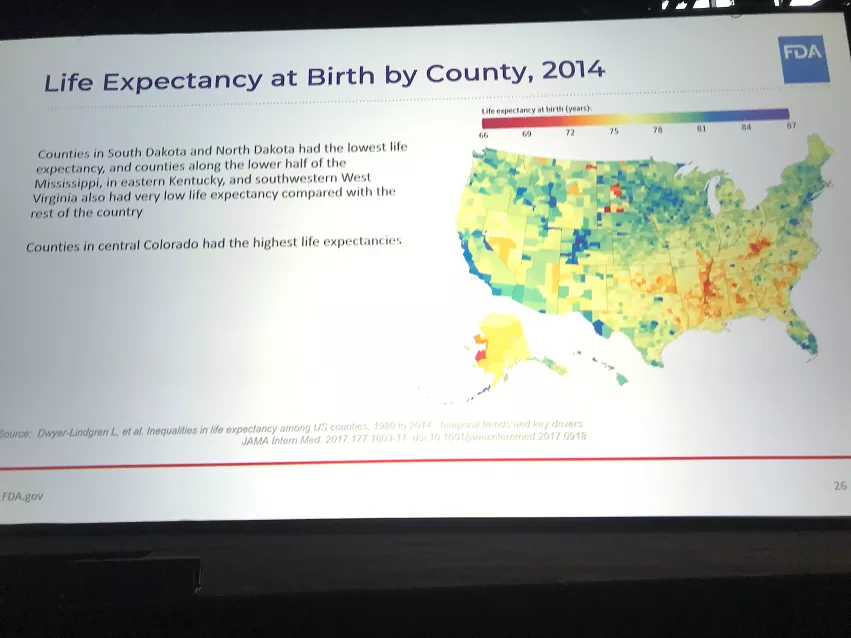
In a map Califf showed of the United States with each county color coded by life expectancy, it was clear people who live in very rural areas had the lowest average life spans. In a chart of rural vs. urban life expectancies from 1970 to 2016, the numbers were about the same for both groups, but in the late 1980s they began to diverge. By 2016, there was about a 20% disparity for rural Americans.
"Life expectancy is an issue, with rural America showing expanding, negative disparities," Califf said. "I think this is the biggest threat we need to address."
He said there needs to be a day of reckoning, where more is done and new ideas are explored by physicians, healthcare systems and the government to address these disparities.
"What we are doing now is not working," he explained.
Califf said the healthcare system needs to address social determinants, focus on solutions that work. These do not have to be high-tech devices, but can even be simple things to boost screening programs and concentrate more on prevention rather than dealing with severely ill patients with advanced disease, where costs are high and outcomes can be poor.
Putting more emphasis on getting patients to quit stop smoking also could be a major driver for improving health. Califf said about 480,000 people die each year in this country due to smoking related illnesses. He said care for these patients and their conditions is about $240 billion a year.
What can be done to address health inequities in the U.S.?
Califf outlined several things physicians and healthcare systems should consider to more the needle on health disparities, including:
• Reinvigorate our evidence generation system so that we know what works and what does not work with less argument.
• Relentlessly focus the system on interventions that work to tackle the major sources off death and premature loss of function.
• Keep the innovation engine stokes for more precision and effective treatment of rare diseases and p[recision medicine
• Focus on the basics of common, non-communicable diseases.
• Spend time every day combating the misinformation.
Physicians need to combat misinformation
Another major problem facing healthcare today is the rampant proliferation of misinformation. Califf said this problem is directly impacting the rise in deaths in the U.S. and causing hospital emergency rooms to be filled. Almost all the current 200-400 patients who are still dying from COVID each day in the U.S. could have been prevented if they had gotten the vaccine.
"If you are up to date on your vaccine and receive anti-virals almost none of those people are dying," Califf explained. "Almost 100% of the people dying today from COVID are not vaccinated."
More recently, there has been a surge in patients presented in emergency rooms across the country for a range of non-COVID respiratory ailments, like the flu and pneumonia. He said vaccines are easily available for both of these diseases, but people have to voluntarily get their shots.
He said vaccination and following medical advice from public health officials and doctors has been called into question the past couple years of the COVID pandemic, and is having continued impact on public health. This is largely due to the right-wing side of the political spectrum in the U.S. turned public health safety and science-driven decision making into political issues. This included political leaders who called into question science- and data-driven health policy decisions, making claims about treatments that were disproven as being ineffective by clinical trials, and turning vaccinations into a political issue rather than trying to address the health emergency.
Califf called on all the clinicians at AHA to make an effort to actively combat the epidemic of misinformation about science and the practice of medicine.
"Spend time every single day combating the misinformation that is contributing to the destruction of our health and well-being," Califf stressed.