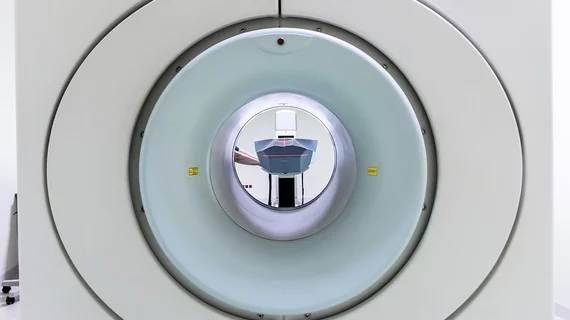
Portable MRIs bring imaging to stroke patients’ bedsides
Research presented at the American Stroke Association’s International Stroke Conference in Los Angeles this February suggests a portable, low-field MRI system may soon improve access to care for patients who have trouble making it to a high-tech facility.
The portable solution could be useful for patients anywhere, though, author Kevin Sheth, MD, of Yale School of Medicine and Yale New Haven Hospital, said in a release—from advanced urban hospitals to remote care facilities to international aid sites. Portable MRIs would also minimize the need for special power supplies and cooling requirements and would lower medical costs.
Sheth and his team tested the low-field approach in 85 stroke patients, 46% of whom experienced ischemic stroke, 34% of whom experienced intracerebral hemorrhage and 20% of whom suffered subarachnoid hemorrhage. All patients received bedside low-field MRI within seven days of symptom onset.
Exam time averaged 30 minutes, and the researchers said that, save five patients who couldn’t fit into the 30-centimeter bore and six who experienced claustrophobia, almost all patients completed the whole exam. There were no significant adverse events.
“We started this research several years ago because obtaining accessible, meaningful brain imaging for patients has been a major worldwide healthcare gap for decades,” Sheth said. “The whole thing works because we are using low-field magnets to acquire brain images after a stroke.”
Sheth said his team is working on improving the image quality of the lower-field MRIs, but the current units do produce clinically useful images. The portable MRIs also don’t interfere with any nearby equipment and eliminate the need to remove metal objects from the room.
“We’ve flipped the concept from having to get patients to the MRI to bringing the MRI to the patients,” Sheth said. “This early work suggests our approach is safe and viable in a complex clinical care environment.
“There’s a lot of work to do, however we’ve cracked the door open for bringing this technology to any setting, anywhere. In rural settings, urban advanced hospitals and in remote villages in areas of the world where it’s hard to get an MRI—not anymore.”