Laser technology may help determine viability of transplant hearts
A new laser imaging technology may be able to determine which donor hearts are viable for transplant and which will result in poor outcomes without the need for coronary angiography or use of contrast agents that can damage an explanted heart.
Severe coronary artery disease (CAD) is a major determinant of primary graft failure and early death after heart transplantation. As donors with extended criteria such as advanced age and cardiovascular comorbidities are routinely allocated for heart transplantation today, screening of hearts has become more important.
With a long waiting list for heart transplants, researchers are looking for ways to screen donated hearts to determine their viability and potential complications is used. While invasive coronary angiography is considered a gold-standard for donor heart evaluations, only about one-third of of donor hearts are examined this way. Ex situ heart perfusion (ESHP) studies can be performed after a donor heart is removed from the donor. This method has found the contrast agent used degrades the heart, and a better method that better preserved the heart has been sought.
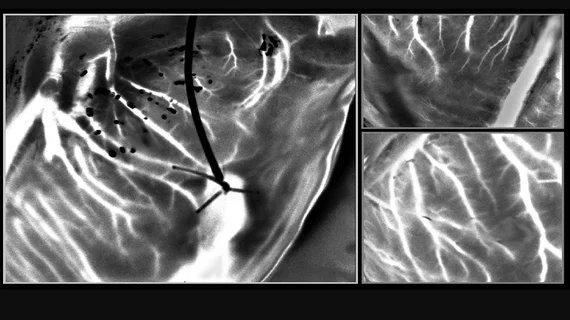
A group of French researchers recently examined use of an imaging technology based on the light scattering to assess the structure and functionality of the cardiac vasculature without the need for contrast. Laser speckle orthogonal contrast imaging (LSOCI) was developed to selectively detect multiple scattering of moving red blood cells. A laser is focused on the donor heart and the backscattered light of moving particles can be observed with a camera, which produces a blurring effect and can act as a contrast between blood vessels and surrounding tissue.
As a full-field optical technique, LSOCI enables the creation of high-resolution imaging of the entire peripheral vasculature of the heart with real-time imaging capabilities. The results of preliminary study were published in the April 2023 issue of the Journal of Biomedical Optics (JBO).[1]
“The optical technique allows high-resolution imaging of the entire peripheral vasculature of the heart in real time,” explained Professor Elise Colin from Paris Saclay University, France, in a statement from the International Society of Optics and Photonics (SPIE). Colin led the team of researchers.
To test this method, the researchers developed a clinical model to study coronary circulation on donor hearts before transplantation. They then used a laser and a camera mounted on an articulated arm fixed above the perfusion module—which contained the donor heart—to generate and analyze rapidly varying speckle patterns. To overcome the challenges in tracking vasculature due to the beating of the heart, the researchers further optimized the technique with a method called multi-period-enhanced signal-to-noise ratio (MPE-SNR). They took a series of images over time to build a set of frames that depicted the vasculature at similar heart positions. Each image in this sequence was then optimized using the other images to reduce noise and enhance details. The optimized image represented the vasculature at a different time point, and the researchers used a sequence of such images to visualize vasculatures as small as 100 microns in a few seconds.
The newly developed imaging technique enables precise visualization of blood circulation. In the future, this technique may potentially identify myocardial perfusion abnormalities that indicate underlying heart conditions, such as coronary artery disease.
“The noncontact technique, based on laser speckle, provides imaging of blood circulation within donor hearts and has important implications for identifying hearts that are safe and suitable for transplantation," said Amy Oldenburg, PhD, professor at the University of North Carolina at Chapel Hill and JBO associate editor, in the SPIE statement.