How monitoring MR can help cardiologists anticipate TAVR outcomes in patients with low-flow, low-gradient AS
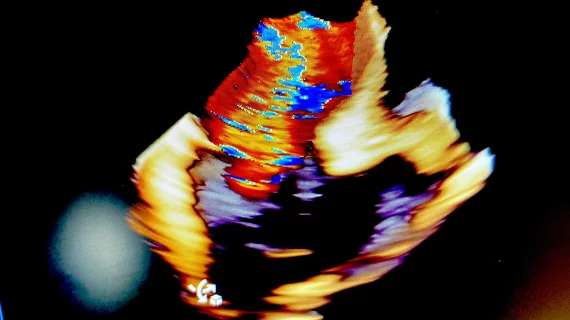
Patients with low-flow, low-gradient aortic stenosis (LFLG-AS) face a heightened risk of poor outcomes after transcatheter aortic valve replacement (TAVR) if they present with severe mitral regurgitation (MR), according to new research published in the Journal of the American Heart Association.[1] In addition, researchers noted, persistent MR after TAVR is a warning sign that the patient may face an especially challenging road to recovery.
“The risk–benefit ratio of patients with LFLG‐AS may be less favorable than in the high‐gradient forms and depends on a proper patient selection by the local heart team,” wrote first author Germano Junior Ferruzzi, MD, an interventional cardiologist with the department of medicine at the University of Salerno in Italy, and colleagues. “Prior studies have investigated the conditions associated with poor outcomes after TAVR in order to optimize procedural candidacy and patient management. However, poor evidence is available in the very‐high‐risk scenario of LFLG‐AS.”
Ferruzzi et al. tracked data from 268 patients with LFLG-AS who underwent TAVR in one of two high-volume facilities in Italy from 2017 to 2022. Twenty-one percent of those patients presented with moderately severe or severe MR.
The study’s primary outcome, the composite of all-cause mortality and heart failure hospitalizations after one year, was seen in 20.5% of patients. All-cause mortality on its own was seen in 10.8% of patients, and heart failure hospitalizations on their own were seen in 12.7%.
Patients with moderately severe or severe MR were associated with a heightened risk of all of these outcomes. This was true even after making certain adjustments or breaking the data down into smaller subgroups.
Another key takeaway from the group’s analysis was the impact of persistent MR following TAVR among LFLG-AS patients. A significant improvement in MR was seen in 44% of patients after TAVR. Patients who did not experience such an improvement were linked to a higher risk of the study’s primary outcome.
“Although related to mechanisms potentially different, the improvement of MR after TAVR was reported both in patients with classical and paradoxical LFLG‐AS forms,” the authors wrote. “In patients with classical LFLG‐AS, it is mainly explained by a reduction in the mitral leaflet tethering area. Conversely, the improvement of MR in patients with paradoxical form is predominantly related to a reduction of hemodynamic afterload.”
Overall, the authors concluded, cardiologists and any other members of the heart team should pay close attention to MR when considering the treatment of patients with LFLG-AS.
“Our study suggests that, in patients with LFLG‐AS undergoing TAVR, the assessment of concomitant MR is of utmost importance not only before the procedure but also after TAVR to identify patients with improvement versus those with persistence of severe MR,” they wrote. “Patients with persistent moderately severe or severe MR should be carefully monitored after discharge and should receive guideline‐directed medical therapy for heart failure, including transcatheter mitral valve replacement, when judged appropriate by the local heart team. However, further studies are warranted to establish the best clinical and therapeutic management of this LFLG‐AS population at persistently high risk despite TAVR treatment.”
Read the full study in the Journal of the American Heart Association here.