Cardiac CT before TAVR detects CAD with high accuracy, suggesting a reduced need for invasive imaging
CT angiography (CTA) is an effective tool for ruling out significant proximal coronary artery disease (CAD) before patients undergo transcatheter aortic valve replacement (TAVR), according to new research out of Cleveland Clinic. Does this mean screening TAVR patients with invasive coronary angiography (ICA) could be a thing of the past?
The study’s authors explored this question, and many others, sharing their findings in JACC: Cardiovascular Interventions.[1]
“To date, evaluation for concomitant CAD is still recommended before TAVR,” wrote Nicholas P. Kondoleon, MD, an internal medicine fellow at Beaumont Health who was with Cleveland Clinic at the time of the trial. “In most cases, this is done with ICA, which comes with its own risks and cost. Current practice guidelines and expert statements recommend screening to rule out significant proximal lesions, and the decision to perform angiography and revascularization is based on individual clinical needs.”
Kondoleon et al. noted that CTA is already used to evaluate the anatomy of TAVR patients. To see if it could screen for signs of significant CAD as well, the group evaluated data from more than 2,200 patients who underwent TAVR at Cleveland Clinic from 2015 to 2021. The mean patient age was 79.2 years old, 53.4% were male and 92.7% were white.
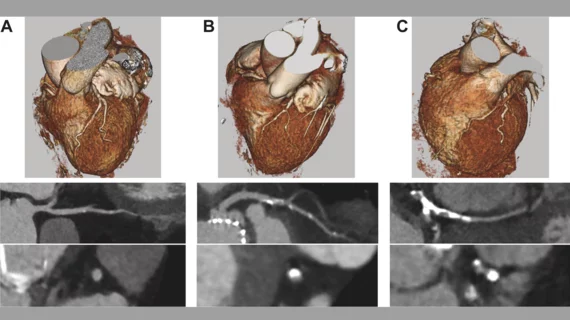
All patients underwent both CTA and ICA before TAVR, but the authors blinded themselves to ICA results to focus on the effectiveness of CTA. CTA coronary reconstruction was used to assess each patient’s left main coronary artery, proximal left anterior descending coronary artery, proximal left circumflex coronary artery, and proximal right coronary artery. At that point, ICA results were reviewed to examine if screening with CTA only provided an accurate snapshot of the patient’s coronary health.
Overall, the authors found that CTA evaluations were associated with a sensitivity of 90%, specificity of 92%, positive predictive value (PPV) of 74% and negative predictive value (NPV) of 97% when detecting stenosis of at least 50%. Those numbers improved to a sensitivity of 91%, specificity of 97%, PPV of 83% and NPV of 99% when detecting stenosis of at least 70%. When identifying graft patency, meanwhile, CTA’s sensitivity was 86%, its specificity was 97%, its PPV was 84% and its NPV was 98%.
In addition, the team performed a Cohen’s kappa analysis that determined the agreement between CTA and ICA was “substantial to near perfect.”
“Although CTA may not be a tool that can guide revascularization, its use has a place in the periprocedural TAVR process in ruling out significant proximal CAD,” the authors wrote. “At our institution, this could have spared 1,148 of 2,217 patients (51.8%) the need for additional invasive testing and the associated risks.”
The group concluded that the consistent use of pre-TAVR screening with CTA “could spare patients the need for additional invasive testing before the procedure.” More research is still needed, however, to further increase the potential impact of noninvasive screening.
Study co-authors from Cleveland Clinic included Samir R. Kapadia, MD; Amar Krishnaswamy, MD; James Yun, MD; Rishi Puri, MD, PhD; and others.
Read the full analysis in JACC: Cardiovascular Interventions here.