Cardiologists may want to rethink how they track prosthesis-patient mismatch after TAVR
Prosthesis-patient mismatch (PPM) is always on the mind of cardiologists before and after they perform transcatheter aortic valve replacement (TAVR). According to new findings published in EuroIntervention, however, there may be more helpful ways to track PPM.[1]
“PPM is a condition in which the effective orifice area (EOA) of a normally functioning prosthesis is too small relative to the patient’s body surface area (BSA), resulting in a high residual transprosthetic pressure gradient,” wrote lead author Daijiro Tomii, MD, a cardiologist with Bern University Hospital in Switzerland, and colleagues. “In surgical series, PPM has been associated with adverse clinical outcomes after surgical aortic valve replacement (SAVR). However, the impact of PPM in the TAVR population remains controversial because of differences in the methods used to ascertain PPM.”
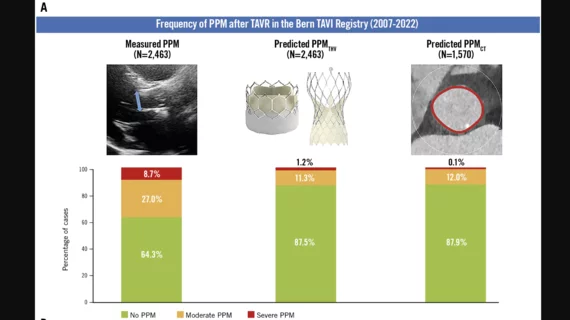
Tomii et al. noted that PPM after TAVR is typically measured by evaluating transthoracic echocardiography (TTE). However, some researchers have suggested this method results in a significant overestimation of the frequency of PPM after TAVR.
Could predicting PPM be a better option? To find out, the group explored the potential of two ways to predict PPM after TAVR. One method, predicted PPMTHV, is based on published EOA reference values for each TAVR valve. Another method, predicted PPMCT, is based on CT measurements of the aortic annulus.
The study included data from nearly 2,500 TAVR patients who were treated with either balloon-expandable or self-expanding devices from August 2007 to June 2022. The mean age of the group was 82 years old. Any patients with incomplete information were excluded from the analysis.
Researchers evaluated measured PPM, predicted PPMTHV and predicted PPMCT for all patients. All measured PPM calculations included TTE data performed by a board-certified cardiologist and echocardiography specialist before and after the procedure. All predicted PPMTHV calculations were made using reference data published by the valve’s vendor. Finally, all predicted PPMCT calculations were made using pre-TAVR CT scans reviewed by trained radiologist.
Overall, the frequency of moderate PPM was 27% using measured PPM, 11.3% using predicted PPMTHV and 12% using predicted PPMCT. The frequency of severe PPM, meanwhile, was 8.7% using measured PPM, 1.2% using PPMTHV and 0.1% using predicted PPMCT.
“The discrepancy in the frequency of PPM according to different definitions relates to inaccuracies in the assessment of EOA,” the authors wrote. These inaccuracies appear to occur for several reasons. One example is that “higher transvalvular gradients and smaller EOAs are documented by Doppler echocardiography compared to cardiac catheterization due to the pressure recovery phenomenon.”
Perhaps the study’s most striking finding was that, after a median follow-up period of 429 days, the authors did not identify an increased risk of 10-year mortality among patients with PPM, no matter how PPM was calculated.
While this suggests that cardiologists relying on the measured PPM technique may want to consider a different approach, the authors did emphasize that it is still too early to make any final decisions about changing practice.
“Further study is needed to evaluate the impact of PPM on long-term clinical outcomes after TAVR in younger patients,” the authors wrote.
Click here to read the study in EuroIntervention.