Day 1 at ACC.24: Late-breakers examine potential new heart attack, heart failure treatments
ACC.24, the annual meeting of the American College of Cardiology (ACC), kicked off on Saturday, April 6, with a series of late-breaking clinical trials focused on testing the safety and effectiveness of new treatment strategies.
RELIEVE-HF: Interatrial shunt treatment among heart failure patients
Gregg Stone, MD, a professor of cardiology and population health sciences at Icahn School of Medicine at Mount Sinai, opened the festivities by presenting findings from RELIEVE-HF, a randomized trial designed to evaluate the safety and effectiveness of treating heart failure patients with an interatrial shunt. Stone et al. randomized more than 500 patients in North America, Europe, Israel, Australia and New Zeeland to either receive the V-Wave Ventura Interatrial Shunt System—a small device designed to reduce pressure on the left atrium and the lungs—or undergo a placebo procedure.
After a median follow-up period of 22 months, the group found that treatment with the V-Wave device was safe, but did not significantly improve cardiovascular outcomes for heart failure patients. Diving deeper into the data, however, the group found that treatment was actually quite beneficial for patients presenting with heart failure with reduced ejection fraction (HFrEF). On the other hand, treatment was potentially harmful for patients presenting with heart failure with preserved ejection fraction (HFpEF).
Researchers also identified an improvement in quality of life (QOL) as measured by Kansas City Cardiomyopathy Questionnaire (KCCQ) scores. Because QOL improved for patients in both the treatment and the placebo groups, Stone and colleagues determined it wasn’t necessarily due to treatment with the V-Wave device.
“There was a tremendous placebo effect,” Stone said. “These observations, especially the fact that quality of life improved in HFpEF patients who were more likely to be hospitalized for heart failure and had reduced survival after shunt treatment, raise questions about the interpretation of this QOL measure in these kinds of trials.”
V-Wave highlighted the improvement seen among HFrEF patients in its own review of the RELIEVE-HF data.
“Between the U.S. and the EU, there are 2-3 million HFrEF patients with New York Heart Association Class III symptoms,” Neal Eigler, MD, V-Wave’s CEO, said in a statement. “These patients have a prognosis worse than many cancers and few remaining options. This places a terrible burden not only on patients but also on their families and the healthcare system. We are excited by the RELIEVE-HF results showing that the Ventura Interatrial Shunt improved heart failure hospitalizations and other study endpoints in patients with HFrEF, suggesting that our investigational device could potentially address those needs.”
EMPACT-MI: Empagliflozin after a heart attack
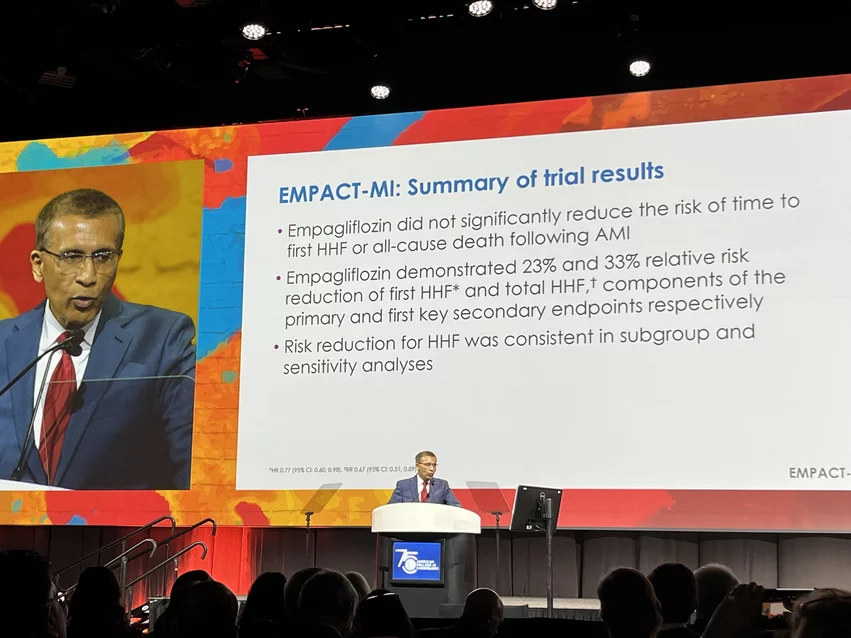
Javed Butler, MD, president of the Baylor Scott and White Research Institute, was up next to present results from the EMPACT-MI randomized trial, which examined treating patients with empagliflozin following a heart attack.
Butler’s team explored data from more than 6,000 acute myocardial infarction (AMI) patients treated with empagliflozin, a popular SGLT-2 inhibitor sold under the brand name Jardiance, or a placebo.
Treatment with empagliflozin did not significantly impact the study’s primary endpoint—the combination of heart failure hospitalizations and all-cause mortality—but it did appear to dramatically improve heart failure hospitalization rates when tracked on their own. For example, patients were 23% less likely to be hospitalized for heart failure for the first time and 33% less likely to experience any heart failure hospitalization if treated with empagliflozin. This risk reduction was consistent among all heart failure subgroups, Butler noted.
“In terms of heart failure outcomes, the data is not only strong, but it’s consistent with what we’ve found over the past 10 years in yet another population,” he said. “This finding is completely consistent in both direction and magnitude with other studies of SGLT-2 inhibitors in populations with diabetes and chronic kidney disease.”
Boehringer Ingelheim and Eli Lilly and Company, the two companies behind empagliflozin, shared their excitement about the EMPACT-MI results.
“These results add to our understanding of SGLT2 inhibitors and contribute to the body of evidence across six clinical studies examining the potential for Jardiance to impact major outcomes in a broad population of adults with heart failure, chronic kidney disease or type 2 diabetes,” Mohamed Eid, MD, MSc, MHA, vice president of clinical development and medical affairs for cardio-renal-metabolic medicine at Boehringer Ingelheim Pharmaceuticals, said in a prepared statement.
“There is still an unmet need to reduce the risk of new onset heart failure and other common complications after a heart attack,” added Jeff Emmick, MD, PhD, senior vice president of product development for Eli Lilly and Company. “However, in adults who have chronic heart failure, Jardiance has proven to be an important therapy for reducing the risk of cardiovascular death and heart failure hospitalizations, and has the potential to meet the needs of millions of people worldwide.”
AEGIS-II: ApoA-1 injections in heart attack patients
C. Michael Gibson, MD, a professor of medicine at Harvard Medical School, took the stage next to discuss a new approach to improving outcomes for AMI patients.
Gibson presented data from AEGIS-II, an international trial that looked at the potential of injecting heart patients with Apolipoprotein A-I (ApoA-1) infusions via the investigational drug CSL112. Because ApoA-1 is a key component of HDL cholesterol, which removes cholesterol from the arteries and helps it exit the body, researchers thought ApoA-1 injections following an AMI could potentially reduce LDL cholesterol and deliver improvements in cardiovascular outcomes.
The team’s research included more than 18,000 patients recruited from a whopping 49 countries. Complete follow-up data was available for 99% of participants. The median patient age was 65.5 years old, 74% of patients were men and 84.5% were white. Each participant was randomized to either receive ApoA-1 infusions or a placebo for four weeks; the first treatment occurred within five days of hospitalization for AMI.
Overall, after 90 days, six months and one year, time to the first occurrence of a major adverse cardiovascular event (MACE) was comparable for the two treatment groups. The infusion group did experience a reduced MACE rate after 90 days (4.8%) compared to the placebo group (5.2%), but that difference was not statistically significant. Gibson also noted that the infusions were safe, an especially crucial detail when considering the potential of a brand new approach to patient care.
Perhaps the biggest takeaway from AEGIS-II was the fact that patients with LDL cholesterol levels of 100 mg/dL or higher saw a 30% reduction in their MACE risk after 90 days. This was statistically significant, Gibson explained during his presentation, but the impact was not at all present for patients with LDL cholesterol levels lower than 100 mg/dL
“Baseline LDL modulated the treatment effect,” Gibson said.
The authors also found that patients in the infusion group were less likely to have repeat myocardial infarction after 180 days and less likely to have a myocardial infarction caused by a blood clot in a stent at 90 days and 180 days.
“Overall, our findings are consistent with ApoA-I having a role in stabilizing heart blockages and reducing the risk of a blockage that ruptures and causing a heart attack further out than 90 days,” Gibson said. “It’s plausible that by giving ApoA-1 to clear the cholesterol out of the body and then treating the patient with cholesterol-lowering medications to keep LDL cholesterol levels low, we could see reductions in deaths and heart attacks that continue over time.”