American College of Cardiology shares new guidance focused on evaluation, management of cardiogenic shock
Cardiogenic shock (CS) is a complex condition to manage, creating challenges for even the most experienced cardiologists. The American College of Cardiology (ACC) published new clinical guidelines to help care teams provide the best care possible when patients present with potential symptoms of CS.
The new document, published in full in the Journal of the American College of Cardiology, represents the ACC’s first Concise Clinical Guidance; it was designed to be an easy-to-use reference for keeping track of a complicated topic. Cardiologist Shashank S. Sinha, MD, MSc, medical director of the cardiac intensive care unit at Inova Fairfax Hospital, served as the chair of the writing committee behind this new guidance. He said Concise Clinical Guidance documents are “highly focused, limited in scope and aim to illustrate clinical decision-making processes using figures, tables and checklists.”
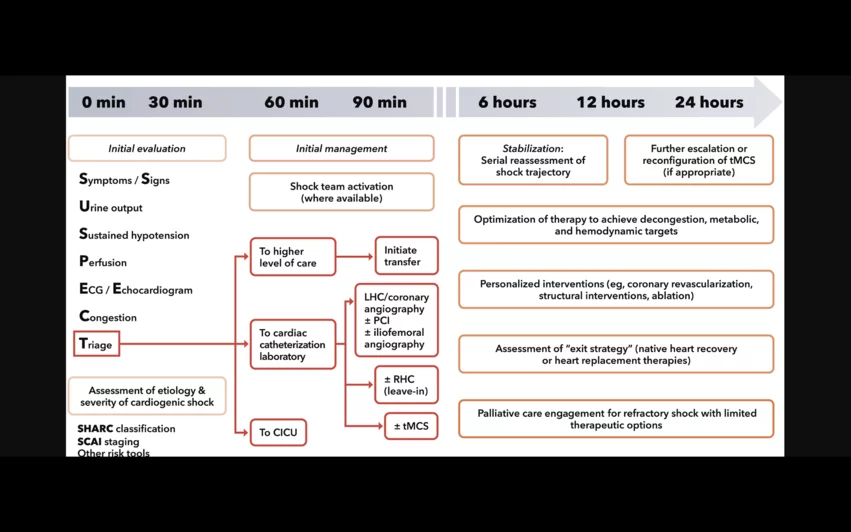
The guidance includes, among other things, one-hour and 24-hour roadmaps, detailed definitions and an updated look at how invasive hemodynamic assessments and noninvasive cardiac imaging modalities can work together to effectively evaluate CS patients. It also covers a helpful mnemonic device, SUSPECT CS, and highlights the importance of shared decision-making when treating these patients.
“CS remains a hemodynamically complex, multifactorial syndrome with high morbidity and mortality,” according to the document. “A high index of suspicion is necessary to promote early recognition, confirm the diagnosis and initiate prompt pharmacological and/or temporary mechanical circulatory support therapy based on risk stratification. Invasive hemodynamic monitoring may be useful in guiding therapy selection and escalation of support. Serial reassessment, particularly within the first 24 hours, is advised to ensure hemodynamic stability, restore tissue perfusion, and mitigate end-organ damage. In this manner, a standardized team-based approach has been associated with improved outcomes and can facilitate the patient’s transition to myocardial recovery, advanced therapies, or palliative care/hospice, as appropriate.”
Click here to read the full guidance.
![A majority of medical devices involved in Class I recalls were never required by the U.S. Food and Drug Administration (FDA) to undergo premarket or postmarket clinical testing, according to new research published in Annals of Internal Medicine.[1]](/sites/default/files/styles/top_stories/public/2024-09/istock-1209664264.jpg.webp?itok=gQInU1vO)