OCT-guided PCI improves survival after life-threatening heart attacks
Using optical coherence tomography (OCT) to guide percutaneous coronary intervention (PCI) procedures is associated with significant long-term benefits for ST-segment elevation myocardial infarction (STEMI) patients compared to angiography alone, according to new findings published in EuroIntervention.[1]
Most prior studies of OCT-guided PCI have focused on patients presenting with stable angina or even non-ST-elevation myocardial infarction (NSTEMI), the authors wrote. Because STEMI is quite different from stable angina or NSTEMI, with patients facing a much higher immediate risk of mortality or other significant adverse events, the group wanted to specifically examine OCT’s potential to benefit STEMI.
The study included nearly 4,000 consecutive STEMI patients who underwent primary PCI from January 2017 to December 2020 at a high-volume academic hospital in China. Patients with cardiogenic shock or preinterventional thrombolysis were excluded, as was anyone evaluated with intravascular ultrasound (IVUS) during PCI.
The mean patient age was 60.2 years old; 71.7% of patients were male and OCT guidance was used for 69.2% of PCI procedures. Angiography alone was used in the remaining 30.8%. Nearly all patients received antiplatelet agents and a statin at discharge. Median follow-up time was 3.5 years.
Patients treated with OCT-guided PCI tended to be younger and were more likely to be male. OCT guidance was less likely in patients presenting with a previous myocardial infarction, diabetes, hypertension or chronic kidney disease. In addition, the authors noted OCT was more common when the culprit vessel was the left anterior descending artery.
Another key takeaway from the group’s work was the reduced rate of drug-eluting stent implantation (62.6% vs. 80.2%) seen when OCT guidance was used. In fact, OCT guidance was associated a lower total number of stents, larger maximum stent diameter and higher rate of post-dilation compared to angiography guidance.
The group also found that the all-cause mortality (10.4% vs. 19%) and cardiovascular mortality (8% vs. 14.1%) rates after five years were both lower in the OCT-guided group. These advantages were also seen after the group performed propensity score matching.
“Instead of employing a one-size-fits-all approach for stent implantation in STEMI, it might be a better paradigm to perform OCT after restoring antegrade blood flow, then making further reperfusion decisions, optimizations and tailored medications according to the comprehensive findings from angiography and OCT,” wrote first author Luping He, MD, a cardiologist with the 2nd Affiliated Hospital of Harbin Medical University and National Key Laboratory of Frigid Zone Cardiovascular Diseases in China, and colleagues.
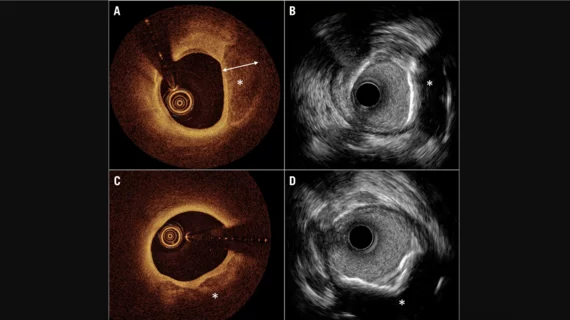
He et al. also compared OCT with IVUS, the other popular intravascular imaging modality interventional cardiologists use to guide PCI.
“Advantages of IVUS include the detection of plaque burden and vascular remodeling,” the group wrote. “However, the diagnosis of thrombus by IVUS is presumptive. OCT is the best way to detect thrombus and the only technique to positively diagnose plaque erosion in vivo, although it cannot see through red blood cell-rich thrombus. These advantages maintain OCT as a promising tool in the management of STEMI”
The full study is available in EuroIntervention, a journal from EuroPCR and the European Association of Percutaneous Cardiovascular Interventions.