OCT-guided PCI boosts outcomes when treating complex lesions
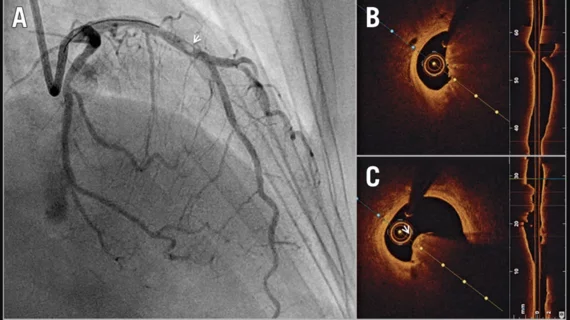
Using optical coherence tomography (OCT) to guide percutaneous coronary intervention (PCI) in patients with complex coronary lesions is associated with a higher likelihood of survival and lower risk of adverse complications than using traditional angiography, according to new data published in The Lancet.[1]
The findings were also presented Monday, Sept. 2, at Europeasn Society of Cardiology (ESC) Congress 2024 in London.
The rise of intravascular imaging-guided PCI has been a significant trend in recent years, with both OCT and intravascular ultrasound gaining momentum among care teams. The American College of Cardiology even recommended intravascular imaging-guided PCI to its members in 2023, and many interventional cardiologists seem to have taken that suggestion to heart.
The OCCUPI trial focused on data from more than 1,600 patients who underwent PCI with a drug-eluting stent from January 2019 to September 2022. All patients presented with complex lesions. The median age was 64 years old, and 80% of patients were men.
Each patient was randomly assigned to undergo OCT-guided PCI or angiography-guided PCI. The study’s primary endpoint—a composite of cardiac death, myocardial infarction, stent thrombosis or ischemia-driven target-vessel revascularization after one year—was seen in 4.6% of OCT-guided PCI patients and 7.4% of angiography-guided PCI patients. Diving deeper into that data, the most dramatic differences were seen in the lower myocardial infarction (0.9% vs. 2.4%) and target-vessel revascularization rates (1.5% vs. 4.1%) between the OCT and angiography groups.
As one may expect, OCT-guided PCI was linked to a longer mean procedure length (53 minutes vs. 43.5 minutes) and using more contrast per patient (300 mL vs. 21 mL) than angiography-guided PCI. Also, the rates of stroke, bleeding events and contrast-induced nephropathy were comparable for the two treatment options.
“Our findings provide more evidence that OCT guidance of PCI procedures in patients with complex lesions has a greater impact on improving their lives than conventional angiography guidance,” lead investigator Byeong-Keuk Kim, MD, a cardiologist with Yonsei University College of Medicine in South Korea, said in a statement. “We now need to establish detailed standard for optimal use of OCT for the improvement of clinical outcomes of PCI for complex cases based on the OCCUPI trial.”
The authors did note that their research had certain limitations. The follow up-period was “relatively short,” for example, and women were underrepresented. In addition, the study’s primary endpoint occurred at a rate lower than the researchers expected. They explained in their analysis that this make their comparisons slightly underpowered.
Click here to read the full study in The Lancet.