Miami cardiologist works to reach more PAD patients in low-income neighborhoods
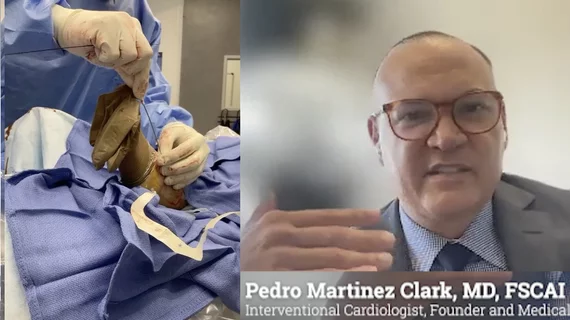
In Miami's low-income neighborhoods, significant barriers prevent residents from accessing proper cardiovascular care. Pedro Martinez-Clark, MD, an interventional cardiologist and founder of Amavita Heart and Vascular Health, sees these issues firsthand, partly from hosting peripheral artery disease (PAD) screenings in these neighborhoods. He spoke to Cardiovascular Business and highlighted how the lack of health literacy, transportation, and financial misunderstandings are the primary factors impeding the delivery of necessary healthcare services.
Martinez-Clark's outreach efforts demonstrate that bridging the gap between healthcare providers and underserved communities requires more than medical expertise. It requires a concerted effort to understand the social and economic factors affecting these populations.
"It might be a transportation issue. They might have a false perception that they might need a procedure that is going to cost a lot of money and be in financial jeopardy and financial distress. And a lot of these patients just don't have the health literacy to understand PAD, or that whatever they're eating might be detrimental to them," he explained.
Addressing health literacy
Martinez-Clark has launched community outreach efforts that focus on PAD screenings. This condition, often undiagnosed in low-income populations, leads to severe complications like critical limb ischemia (CLI). He said many patients do not recognize early symptoms, such as wounds that don’t heal or black spots on their toes, which can lead to amputation if left untreated.
When you explain the use of a simple ankle brachial index test to measure blood flow in the legs and check for PAD, he said patients do not understand what you are looking for. That is when you can show a patient how it works and gain trust and buy-in to impact their health decisions.
"Once you show them, 'look at this waveform,' and you explain to the patient and show them the waveform that is blunted, they're like, 'oh my God, yeah, I see that.' And that gives you more tools to be able to convince the patient that they have to modify their lifestyle or be more present with and interact more with the healthcare provider," he said.
Another barrier regarding health literacy has been patients not understanding what their insurance or Medicare or Medicaid covers. A significant portion of the issues where patient do not get treated is not because they lack insurance, it is because they do not understand what is and is not paid for. “Patients often fear that undergoing necessary procedures will put them in financial jeopardy,” Martinez-Clark explained.
He said Catholic Health Services has been a valuable community partner for outreach programs because they help facilitate access to some minority populations in lower-income areas and because the group works to educate the community about their insurance.
Lack of transportation to make doctor appointments
Beyond the lack of education, transportation is another barrier that causes health disparities. He said many people cannot make it to their appointments because they don’t have a way to get there, so the practice offers free van transport for patients. He said that is a simple solution to one of the big barriers to care.
Mistrust of physicians and language barriers cause health disparities
Martinez-Clark emphasized the importance of community engagement in breaking down these barriers. By partnering with local leaders, especially in the Haitian and Latino communities in the Miami area, his team has gained trust and been able to bring healthcare directly to these underserved populations.
When it comes to mistrust of the healthcare system, especially among minority populations, he acknowledges this is a real obstacle. His strategy involves collaborating with organizations like Catholic Health Services and senior citizen advocacy groups, which already have established relationships in the community.
"So that's been very successful relying on the community leaders to be able to gain access to those communities. If you just show up in a suit, there might be a little mistrust," Martinez-Clark explained
Language barriers are also an issue in Miami, where a sizable number of patients only speak Spanish and many Haiti immigrants only speak Creole. He said they tackled this barrier by having bilingual staff at the clinic.
Watch a video of Pedro Martinez Clark, MD, explain more details about the peripheral artery disease screening programs he runs — Addressing high PAD and CLI rates in Latin and Haitian communities of Miami.