AHA issues a scientific statement on COVID-19 cardiac arrhythmias
Cardiac arrhythmias are common in patients with COVID-19 infections and during recovery, which prompted a new scientific statement from the American Heart Association (AHA) to be published Oct. 14. It offers consensus on the implications for clinical practice, gaps in knowledge and future directions research.[1]
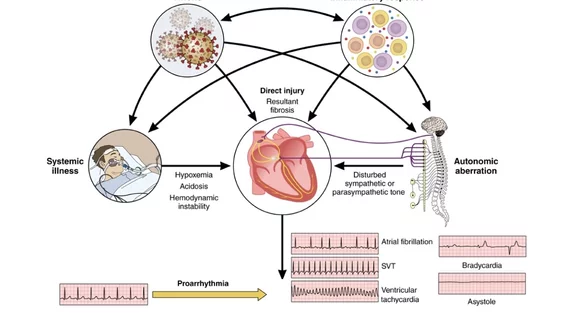
SARS-CoV-2 can cause arrhythmic manifestations that span the risk spectrum from benign to life-threatening. Although the cause has been researched since the start of the pandemic in 2020, the specific pathophysiological mechanisms causing these arrhythmias are not well understood. Researchers said direct viral invasion, changes in autonomic tone, hypoxemia, inflammation and immune-mediated phenomena have been implicated.
The statement covers specific arrhythmias associated with COVID-19, including bradycardia, atrial fibrillation, ventricular tachyarrhythmias and sudden cardiac death. The authors of the study said there is still debate on the impact and exacerbated arrhythmias on the acute and recovery phases of the illness.
"COVID-19 and COVID-19 vaccine–associated myocardial inflammation and autonomic disruption remain concerns. As the pandemic has transformed to an endemic, with discovery of new SARS-CoV-2 variants, updated vaccines, and potent antiviral drugs, vigilance for COVID-19 associated arrhythmic and dysautonomic manifestations remains," the authors wrote.
The objective of the AHA scientific statement is to review the available evidence on the epidemiology, pathophysiology, clinical presentation, and management of cardiac arrhythmias and autonomic dysfunction to provide evidence-based guidance.
The statement includes several highlights:
• Review of the specific arrhythmias associated with COVID-19.
• There are significant drug interactions between nirmatrelvir-ritonavir (Paxlovid) antiviral medication used to treat COVID-19, and cardiovascular medications. This includes interceptions with antiarrhythmic and anticoagulant medications, as well as antibiotics and anti-inflammatory medications.
• How to best manage myocarditis caused by COVID-19 infection. The statement says it is not frequent, but is associated with an adverse prognosis. Myocarditis can also be associated with COVID-19 vaccine in rare cases, but generally has a good prognosis.
• Clinically stable and ambulatory COVID-positive individuals are at substantially less risk than those with severe infections.
• Arrhythmia management should be based on published evidence-based guidelines, with special consideration for the severity of COVID-19 infection, the concomitant use of antimicrobial and anti-inflammatory drugs, and the transient nature of some arrhythmias.
• There is currently no consistent evidence to demonstrate a heightened risk of arrhythmia or sudden death attributable to COVID-19 vaccination in the general population.
• Common symptoms associated with autonomic dysfunction that develops weeks or months after COVID infection, known as post-acute sequelae of SARS-CoV-2 (PASC). This includes fatigue, shortness of breath, palpitations and cognitive dysfunction.
"There is a need to better characterize the presence and severity of autonomic dysfunction in patients with PASC through more consistent and standardized autonomic testing. The pathophysiology, short- and long-term consequences, and effective treatment for PASC-AD require more investigation, because studies performed thus far have been inconclusive and do not provide guidance," wrote Rakesh Gopinathannair, MD, MA, FAHA, director cardiac electrophysiology, Kansas City Heart Rhythm Institute, and chair of the writing committee for the American Heart Association Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology.
According to the World Health Organization (WHO), there have been more than 776 million cases of COVID-19 worldwide since 2020, and new variants are still arising.