TAVR linked to better outcomes than surgery for women, pooled analysis confirms
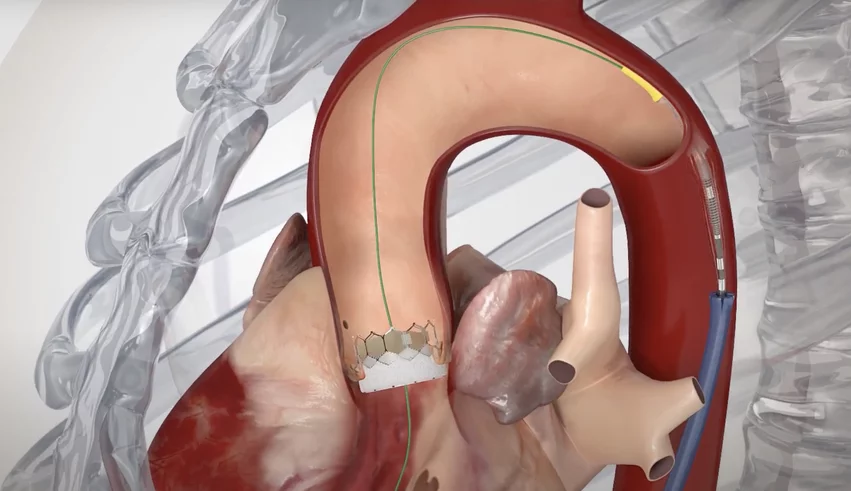
Transcatheter aortic valve replacement (TAVR) with a balloon-expandable transcatheter heart valve is safer and more effective than surgery for women with symptomatic, severe aortic stenosis, according to a new pooled analysis presented at TCT 2024 in Washington, D.C.
Didier Tchétché, MD, an interventional cardiologist and head of the structural heart disease program at Clinique Pasteur in Toulouse, France, and colleagues combined data from the RHEIA and PARTNER 3 trials into a single comparison of TAVR outcomes in female patients.
The RHEIA trial, originally presented at ESC Congress 2024 in London, included data from more than 400 women randomized to undergo TAVR or surgical aortic valve replacement (SAVR) at one of 48 European facilities. It is believed to be the first TAVR trial of its size to exclusively enroll female patients.
The PARTNER 3 trial, meanwhile, was first published in 2019 in The New England Journal of Medicine.[1] It focused on 1,000 low-risk patients with severe aortic stenosis randomized to either undergo TAVR or SAVR, and 32.5% of those patients were women.
Tchétché et al. combined the two trials, comparing 376 women treated with TAVR to 376 women treated with SAVR. All TAVR patients were treated using a balloon-expandable Sapien 3 or Sapien 3 Ultra transcatheter heart valve from Edwards Lifesciences. The mean age for both groups was approximately 73 years old, and the mean Society of Thoracic Surgeons risk score for both groups was 2.1.
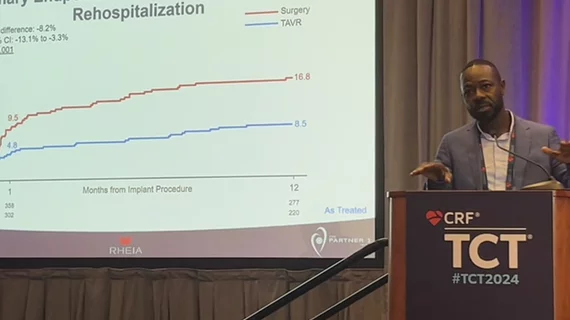
Overall, TAVR was consistently associated with a superior performance when compared to SAVR. The study’s primary endpoint—a composite of all-cause mortality, all-cause stroke and rehospitalization after one year—was seen in 8.5% of TAVR patients compared to 16.8% of SAVR patients. This was driven primarily by the significant difference in rehospitalizations after one year: 5.4% for TAVR and 11.9% for SAVR.
Tchétché did note that mild paravalvular aortic regurgitation (AR) was more likely at one year after TAVR (19.5%) than SAVR (1.8%), but moderate AR was not an issue for either treatment strategy. Also, TAVR was associated with “excellent” hemodynamics and echo assessments, including an aortic valve mean gradient of 14.5 mmHG at one year.
“In women with symptomatic, severe aortic stenosis, TAVR with a balloon-expandable platform could—and this is just a hypothesis—be a preferred treatment option over surgery,” Tchétché said.
Anna Sonia Petronio, MD, an interventional cardiologist and chief of the cath lab at the University of Pisa in Italy, was on hand for Tchetche’s presentation. She emphasized how much safer it can be to treat women with severe AS using an interventional approach.
“It is not easy to go through surgery for patients with a small annulus,” she said. “TAVR is a good option, and probably the best one, for an elderly woman. I think this is a very important trial in the end, and it’s nice to see the merging of these two trials together.”