‘A huge win’: CMS significantly increases Medicare payments for cardiac CT
The Centers for Medicare and Medicaid Services (CMS) has finalized a new payment policy that more than doubles the Medicare reimbursements hospitals receive for performing coronary computed tomography angiography (CCTA) exams.
Under its new 2025 Medicare Hospital Outpatient Prospective Payment System, CMS moved CCTA into a higher ambulatory payment classification (APC). CCTA revenue codes 75572, 75573 and 75574 all now fall under APC 5572.
This update raised the CCTA payment rate from $175 all the way to $357.13.
‘This small coding adjustment creates large ripples of impact’
CCTA utilization is expected to skyrocket throughout the United States now that the payment rate has increased. One medical society is already celebrating the news.
“We’re thrilled with the CMS’s ruling, which better aligns with the cost of providing CCTA services,” Ahmad Slim, MD, chair of the Society of Cardiovascular Computed Tomography (SCCT) Health Policy and Practice Committee, said in a statement. “This is a huge win for U.S. providers as well as the entire cardiac imaging community, ultimately improving patient access to this essential diagnostic tool, which aligns with the society’s overall mission.”
SCCT, the American College of Cardiology (ACC) and other medical societies have been advocating for improvements in CCTA payment rates for years. SCCT has been especially active, emphasizing the improvements this means for patients who may present with suspected coronary artery disease (CAD) and could benefit from additional medical imaging exams.
When CMS first proposed higher CCTA payment rates to see how stakeholders would react, SCCT and the ACC both called on their members to message CMS and show support for the proposal.
“We extend our heartfelt gratitude to the entire cardiovascular imaging community for their efforts and contributions,” Slim said. “This small coding adjustment creates large ripples of impact, alleviating financial pressure on struggling medical practices and potentially expanding cardiac CT testing at more sites across the country, ensuring better patient access to this cost-efficient exam. Every contributing voice was an asset to this advancement forward.”
The SCCT statement also included recommendations for hospitals hoping to get the most out of the elevated APC for CCTA.
“Hospitals should use the cardiology revenue code (0480) for CCTA services, when appropriate,” the group said. “Revenue cycle and billing departments should ensure that systems are updated to reflect the new APC and revenue code usage. Hospitals are encouraged to verify compliance with their Medicare Administrative Coordinator to ensure appropriate billing under the new rules.”
Click here for an exclusive video interview focused on this very topic with Ron Blankstein, MD, a former SCCT president.
HeartFlow cheers reimbursement increases
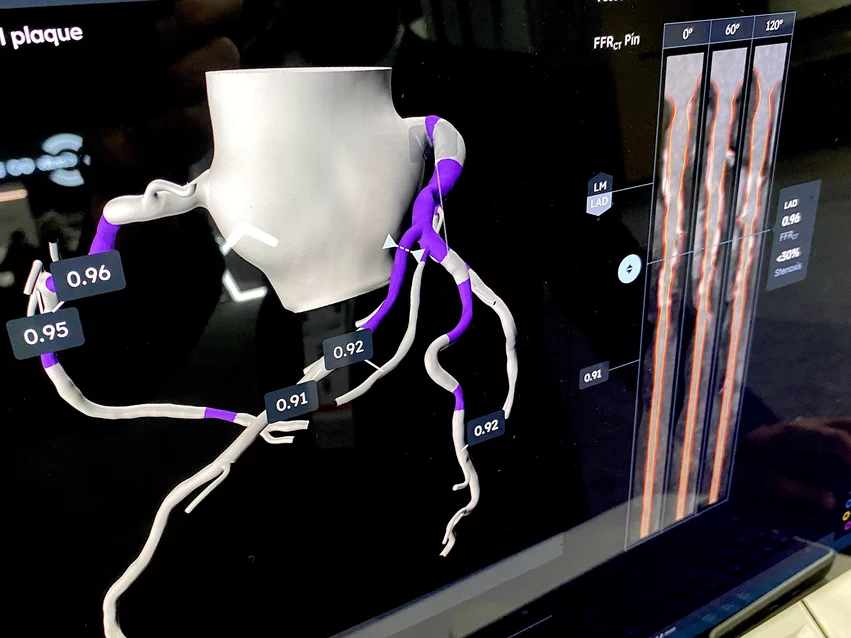
HeartFlow, the California-based healthcare technology company known for its non-invasive AI technologies, issued its own statement highlighting the impact of this update. CCTA images are at the center of the company’s advanced AI offerings, including FFRCT Analysis and Plaque Analysis.
“These substantial reimbursement increases from CMS and coverage policies support what HeartFlow and many physicians and institutions have known—CCTA is the future of CAD diagnostics and is a critically important guideline-recommended test for patients with suspected CAD,” explained Campbell Rogers, MD, HeartFlow’s chief medical officer.
There are additional reasons for HeartFlow to be excited. CMS also announced that the Physician Fee Schedule global payment for CCTA increased to $318, for example, and the payment rate for FFRCT Analysis increased from $997 to $1,017. The payment rate for AI-enabled coronary plaque assessments such as Plaque Analysis, meanwhile, will be set at $950.
These announcements all come just weeks after Plaque Analysis received improved Medicare coverage as a result of a new local coverage determinations approved by a total of five of seven Medicare Administrative Contractors. Also, the American Medical Association (AMA) recently issued a new Category I CPT code that covers the same software. Category I CPT codes are permanent and are only used for established medical procedures, technologies and services.
“We thank SCCT and the American Colleges of Cardiology and Radiology along with the cardiac imaging community for supporting these important increases in reimbursement rates, which will further incentivize clinicians to use this pathway,” Rogers added. “A CCTA pathway combined with HeartFlow FFRCT and HeartFlow Plaque Analysis gives physicians the most comprehensive information for diagnosing and managing CAD.”
Physicians less excited about other CMS policy updates
CMS also issued its final rule for the 2025 Physician Fee Schedule, which included a conversion factor reduction of 2.8%. The American Medical Association and Medical Group Management Association both issued statements of disappointment over the news, urging policymakers in Congress to help stop the reduction from going into effect.