CMS could increase CCTA payments—the American College of Cardiology wants to help
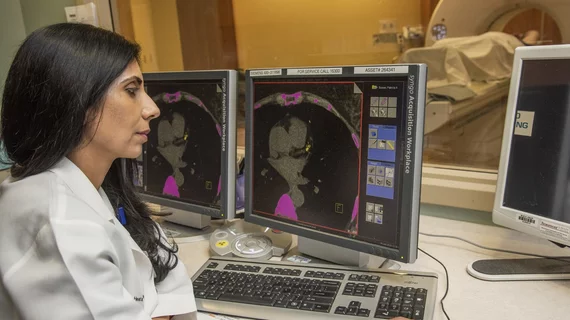
The U.S. Centers for Medicare and Medicaid Services (CMS) recently proposed a new policy that would more than double the reimbursement payments hospitals receive when performing coronary computed tomography angiography (CCTA). Now, the American College of Cardiology (ACC) is joining the Society of Cardiovascular Computed Tomography (SCCT) and others to urge cardiologists and other cardiology professionals to show support for the proposal.
The CMS proposal to boost CCTA payments
CMS included the idea—which allows CCTA to be reported as a cardiology service and could increase Medicare reimbursements from $175 to $386—in its 2025 Hospital Outpatient Prospective Payment System proposed rule.
In addition, CMS has asked multiple questions related to this potential change:
- Where are cardiac CT services performed in a hospital? In the cardiology department, radiology department or elsewhere?
- What determines the revenue codes used for these services?
- What revenue codes are being used for these services in 2024?
CMS is now seeking feedback on the proposal as well as the additional questions. The comment period closes Sept. 9.
The American College of Cardiology responds
SCCT already called for its members to respond to these questions, and now the ACC has done the same thing. The group even provided a letter template for interested parties to fill out and then send on to CMS.
“The ACC, in concert with the SCCT, has raised concerns about the additional costs of cardiac CT over thoracic CT for years,” the ACC said in a message to its members. “The billing change and subsequent questions from CMS present an opportunity to inform future changes to cardiac CT payment. The college will submit formal comments in response to these questions and urge CMS to make a change in payment in the final rule based on their modeling.”
Additional context—and why cardiology and radiology should join forces
Ron Blankstein, MD, associate director of cardiovascular imaging and director of cardiac CT at Brigham and Women’s Hospital and a professor of medicine and radiology at Harvard Medical School, discussed the CMS proposal in a video interview with Cardiovascular Business.
Blankstein, a former SCCT president, noted that hospitals have always received unreasonably low payments from CMS for performing CCTA exams. CCTA requires modern equipment and patient monitoring, but it is still reimbursed at a rate comparable to traditional hand X-rays.
He also emphasized that cardiologists and radiologists should work together to show CMS that this proposal could make a significant impact on patient care.
“All of us need to work together on improving the reimbursement for this,” he said.