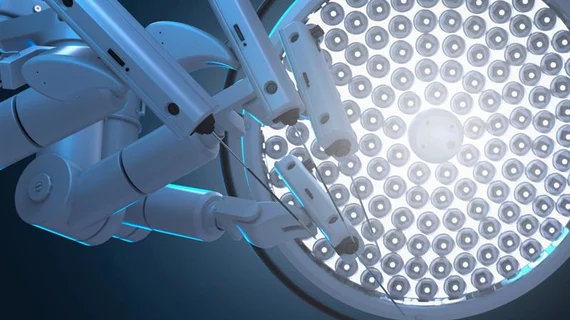
How robotic-assisted mitral valve repair compares to conventional surgery
Robotic-assisted mitral valve (MV) repair is associated with short-term outcomes comparable to more conventional surgical treatments, according to new data published in The Annals of Thoracic Surgery.[1] Overall costs are higher when using robotic guidance, researchers noted, but the difference is relatively low for high-volume facilities.
“Given the relevance of value-based healthcare delivery, costs of new technologies are weighted against their incremental clinical benefit,” wrote first author Joseph Hadaya, MD, PhD, a researcher with the division of cardiac surgery at the University of California, Los Angeles, and colleagues. “In the case of robotic surgery, costs stem from acquisition/maintenance of robotic platforms, disposable instruments, and increased operative times. Some have argued that enhanced recovery and reduced hospitalization time counterbalance the excess costs associated with robotic approaches. Although examined for other operations studies evaluating the costs of robotic MV repair against conventional surgery at the national level are lacking.”
Hadaya et al. explored data from the Nationwide Readmissions Database, focusing on more than 40,000 patients who underwent elective MV repair from 2016 to 2020. Nearly 10% of those patients were treated with robotic-assisted MV procedures. The mean patient age for both groups was approximately 61.5 years old, and a majority of both groups were men. Patients in the MV repair group were linked to a slightly lower Elixhauser Comorbidity Index, which measures disease burden and comorbidity severity.
Evaluation of sort-term patient outcomes
In-hospital mortality rates were similar between robotic-assisted MV repair (0.7%) and conventional surgery (0.8%). Robotic-assisted procedures resulted in lower rates of pulmonary complications (6.1% vs. 8.1%), infection (1.7% vs. 3.4%) and acute kidney injury (5.7% vs. 8.5%), and the rates of stroke, blood transfusion, reoperation and hospital readmission were all comparable. In addition, the odds were much higher of being discharged and sent straight home were significantly higher for patients treated with robotic-assisted MV repair.
After making certain risk adjustments, there was “no association” between the treatment choice and mortality or any other significant complication. The most noteworthy difference after adjustments was the reduced odds of a non-home discharge for patients treated with robotic-assisted MV repair.
“Notably, in our analysis, patients undergoing robotic-assisted surgery were more frequently discharged home rather than to a skilled nursing or rehabilitation facility, which may offset the costs of post-discharge care,” the authors wrote. “Future studies should focus on activity-based costing and post-discharge care utilization for a more nuanced cost-benefit analyses of robotic-assisted cardiac surgery. Given the relevance of value-based healthcare delivery, which can be conceptually defined as the ratio of quality to costs, further studies integrating both quality and cost analyses for mitral valve surgery are necessary.”
Another key takeaway from the group’s analysis: robotic-assisted MV repair was associated with significantly shorter lengths of stay, trimming a full day off of the average hospitalization.
Tracking healthcare costs for robotic-assisted MV repair and traditional surgery
As one may expect, robotic-assisted procedures were linked to significantly higher healthcare costs, even with the shorter lengths of stay. The mean and median costs for robotic-assisted MV repair were $53,600 and $46,800, respectively, while the mean and median costs for traditional surgery were $45,200 and $38,500. The technology involved with robotic-assisted treatment and the longer operative times were the primary drivers of that cost difference, though patient factors—certain comorbidities, for instance—also played a role.
Hadaya and colleagues noted that risk-adjusted costs were less of an issue for high-volume centers. In fact, when focused exclusively on facilities that perform the most MV repair procedures in a given year, the difference in costs was no longer statistically significant.
“High-volume MV repair centers may have improved patient selection protocols, more efficient operating room practices, and expedited care pathways,” the authors wrote. “Furthermore, high-volume centers may distribute fixed costs across a wider group of patients, thereby reducing costs at the individual level. Identification of the mechanisms by which high-volume programs mitigate costs and dissemination of these practices, may reduce the costs of robotic-assisted surgery and aid in development of high quality, cost-effective programs.”
High-volume centers were not associated with better or worse patient outcomes, the team added, though stroke and pulmonary complications were more likely at centers with the lowest volumes.
The researchers called for more research into the “cost-volume relationship” to help inform treatment decisions in the years ahead as this advanced robotics technology continues to evolve.
Click here for the full analysis.