Off-label TAVR for native aortic regurgitation linked to worse outcomes
Treating native aortic regurgitation (AR) with transcatheter aortic valve replacement (TAVR) valves built to treat aortic stenosis (AS) is associated with significantly worse incomes, including a higher risk of death, than using devices specifically designed to treat AR, according to a new meta-analysis published in JACC: Cardiovascular Interventions.[1]
“There are anatomical challenges associated with TAVR for pure AR, including a large annulus, aortic root dilation, lack of leaflet calcium to enable anchoring the valve, and severe regurgitant jet leading to potentially unstable valve positioning and risk of valve embolization,” wrote first author Sahar Samimi, MD, a postdoctoral research fellow with the Houston Methodist DeBakey Heart and Vascular Center, and colleagues. “Recent studies have reported high rates of complications and reintervention associated with treating noncalcified AR with transcatheter heart valves that are designed to treat AS.”
To learn more, Samimi et al. tracked data from 34 different studies, including 19 conducted across multiple treatment sites. All patients included in the group’s meta-analysis presented with pure native AR, but not significant AS.
Comparing JenaValve and JC Medical TAVR valves to off-label devices
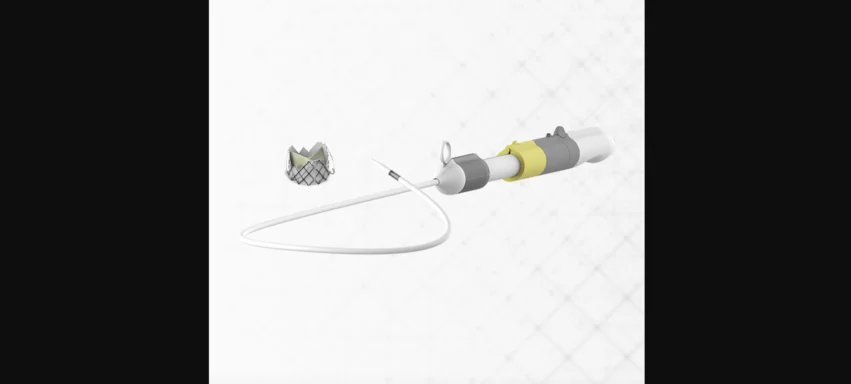
Researchers compared outcomes from patients treated with two TAVR devices specifically designed with AR in mind—the JenaValve Trilogy valve from JenaValve Technology and the J-Valve from JC Medical—and patients who received off-label treatment with a TAVR device for AS.
Both the JenaValve Trilogy valve and the J-Valve are now owned by Edward Lifesciences. The company acquired JenaValve back in July and then acquired JC Medical in August. One important note: Both the JenaValve Trilogy valve and the J-Valve are still only approved for investigational use in the United States. Neither device has received full U.S. Food and Drug Administration approval.
Overall, this study included 2,162 patients with pure native AR. The mean age was 75.4 years old, 57.2% were men and the mean Society of Thoracic Surgeons risk score was 5.6. While 55.2% of patients were treated with a TAVR valve dedicated to treating AR, the other 44.8% were treated with an off-label device.
After 30 days, the estimated all-cause mortality rate for all patients was 4%. This included a 3% all-cause mortality rate for patients treated with JenaValve/J-Valve devices and a 9% all-cause mortality rate for patients treated with off-label devices. Dedicated devices were also associated with an improved success rate (93% vs. 82%), fewer permanent pacemakers (PPMs) (11% vs. 20%), fewer major bleeding events (3% vs. 7%), a lower risk of reintervention and lower risk of moderate or severe residual AR compared to the off-label devices.
In addition, all-cause mortality after one year was 6% for the dedicated devices and 24% for the off-label devices. Post-TAVR strokes and vascular complications were seen at comparable rates in the two groups.
Another perspective: JenaValve Trilogy vs. J-Valve
The study’s authors also performed a separate analysis focused on 588 patients treated with a JenaValve valve and another 605 treated with the JC Medical valve. Key findings included JenaValve patients being associated with a much lower PPM rate (6% vs. 21%) after 30 days and fewer patients presenting with moderate or severe residual AR. These findings, the authors noted, “emphasize the importance of balancing the benefits and risks of different valve designs.”
Final thoughts on treating native AR with off-label devices
“JenaValve and J-Valve have introduced design changes that navigate the challenges of TAVR in native AR, such as fixation mechanisms that securely clasp onto the leaflets, ensuring enhanced anchoring,” the authors wrote. “Our study highlights the potential utility of these valves, demonstrating higher device success and marked reduction in the incidence of moderate or severe residual AR and transcatheter heart valve embolization and migration as well as a decreased need for reinterventions among patients treated with these valves compared with those receiving off-label valves.”
The group concluded that their meta-analysis “support the use of dedicated devices over off-label transcatheter heart valves in fulfilling an unmet need in this high surgical risk population with pure native AR.”
Click here to read the full study in JACC: Cardiovascular Interventions, an American College of Cardiology journal.