TAVR valve improvements may have helped reduce the impact of paravalvular leak
Significant paravalvular leak (PVL) after transcatheter aortic valve replacement (TAVR) may not be as harmful when using contemporary transcatheter heart valves as it was in the past, according to new research published in the Journal of Clinical Medicine.[1]
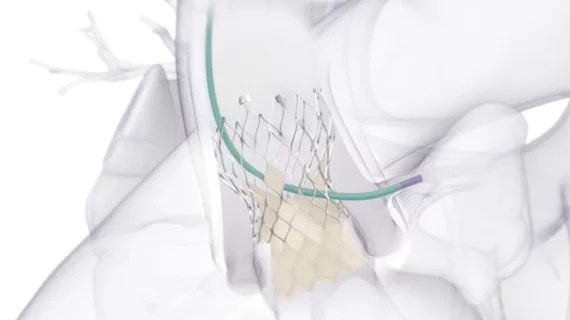
Multiple studies over the years have linked PVL to an increased risk of adverse outcomes, researchers noted, but many modern TAVR valves were designed to help limit PVL. The group hoped to gain an updated look at how often PVL occurs as well as its impact on post-TAVR patient outcomes.
“Nowadays, the indication for TAVR is expanding to younger and lower-risk patient groups,” wrote first author,” Cristina Aurigemma, an interventional cardiologist with Fondazione Policlinico Universitario Agostino Gemelli in Italy, and colleagues. “Therefore, it is essential to consistently evaluate the long-term outcomes of this percutaneous treatment for aortic stenosis (AS).”
This latest analysis included data from 2,125 patients with severe AS who underwent transfemoral TAVR from December 2016 to September 2018 at one of 25 facilities in Italy. All data came from the OBSERVANT II nationwide registry. TAVR patients were treated with contemporary TAVR valves from Medtronic (Evolut R and Evolut Pro) , Edwards Lifesciences (Sapien 3 Ultra) or Boston Scientific (Acurate and Lotus).
Overall, imaging-confirmed significant PVL—meaning either moderate or severe—was seen in 7% of patients after TAVR. Severe PVL was seen in just 0.3% of patients.
The mean ages were 83.4 years old for patients with significant PVL and 82.1 years old for all other patients. Patients with significant PVL were more likely to have presented with a history of peripheral artery disease or previous percutaneous coronary intervention.
In addition, significant PVL was seen in 28.5% of patients with a self-expanding TAVR valve and 8.4% of patients with a balloon-expandable valve. Valve post-dilation was much more common in patients with significant PVL, the researchers added, and valve migration occurred more frequently in patients with significant PVL.
The mean follow-up period for these patients was 3.7 years in total and 4.8 years for patients who were alive at the end of the study. Overall, the study’s primary endpoint—major adverse cardiac and cerebrovascular events after five years—was not significantly higher for patients with significant PVL than patients without significant PVL. On a similar note, PVL did not appear to impact five-year mortality or the risk of being hospitalized for heart failure.
Reviewing these data, researchers wrote that moderate and severe PVL after TAVR made “no clinical impact” on patient outcomes after five years. However, the group did emphasize the importance of technique, specifically pointing to the relationship between post-dilation and PVL.
“The higher prevalence of post-dilation in cases with significant PVL underscores the importance of procedural optimization,” the authors wrote. “Advanced imaging techniques, such as pre-procedural computed tomography, alongside precise valve positioning and deployment strategies, are essential for minimizing PVL. These techniques help to improve annular sizing, optimize prosthesis expansion, and ensure appropriate sealing, thereby reducing the need for corrective interventions such as post-dilation.”
The group did review certain limitations with its research, including its observational nature and the fact that their registry data did not included information related to aortic annulus and leaflet calcifications.
Click here for the full study.